Dr Iain Cranston let’s us know about future improvements
Many months ago Dr Kar from Portsmouth’s QA hospital tweeted a question to the diabetes online community to see if there was any interest in an idea he (or his team) had: would people like the opportunity to meet with healthcare professionals outside of the normal setting, asking questions openly and receiving open answers.
The response was positive, especially from me, and the QA team set up organising the event.
Why?
The need for an event like this was clear to me: it would give a chance to speak openly with professionals who don’t have a defined set of questions to get answers to, or things they have to inform us about. I could ask those questions which seemed silly to me, the sort of things I don’t want to waste anyone’s time over, the sort of thing I would definitely not call the clinic about.
Clearly others felt similar things.
Progress, announcement, sadness, happiness
I’d been following the discussion about the SweetMeet before my Twitter friend Laura even put that name forward. I was excited about attending, along with Amy.
The announcement came out that it was on the 11th May and was open to any type 1 diabetics…who were over 17.
Darn it, Amy’s only 12, I can’t go.
I wished Dr Kar luck but said it was shame I wouldn’t be able to go and he replied by saying he had the power to break the rules for certain individuals.
Great, we’re in, I was happy again.
A simple terms of reference
Initially it was difficult to figure out what the event would be like until Dr Kar coined the phrase “Speed Dating With The Professionals”.
Now it all made sense.
The mention of free bacon sandwiches smoothed the way for many I suspect.
The layout of the morning was set as follows:
– welcome & introduction by Dr Kar
– a speech about patient experience by my friend Laura Cleverly
– speed dating with the professionals
– a speech by Dr Cranston about what’s on the horizon for type 1 diabetes
– an open forum with Lisa Skinner, Diabetes Nurse Specialist
The funny moment of trying to register
When trying to register for the event I called and spoke to a lady who took my details.
“Your name?”. I gave it.
“Your address?”. I gave it.
“Can I just check that you’re over 17 and have type 1 diabetes?”. “Erm, well actually no, but I’m allowed to come, just put me down and ask Dr Kar.”.
“Erm, okay” she said.
The event starts
Driving to the event today Amy and I wrote down as many questions as we could, just in case we got the opportunity to ask them.
Arriving this morning we registered and met with Laura and quickly found the bacon rolls, mmmmm bacon!
We looked at the stands and happened across the one run by the widwife team. “Okay, Amy we don’t need to worry about this for a little while”. Instead of moving on we had a really good chat with the two midwives there.
Ladies and Gentlemen take your seats
It was time to take our seats and when walking into the room we headed to the back only to be greeted by a “hello Kev, what are you doing here?”. It was a guy from work, a guy who I see often, a guy I’ve played football with for years, a guy who had type 1 diabetes, yet I never knew.
It was great to bump into him and have a great long chat about diabetes care, pumps and stuff.
Intro by Dr Kar
Dr Kar is an eloquent speaker, a great advocate of good service by his team and someone who could literally talk for Britain, but in a nice way. He’s so enthuastic about being able to work together (patients and professionals) and shape the future together that listening to him talk about it makes you feel so positive.
He spoke about how the event came about, the ideas, the desires and then he passed over to Laura.
Laura’s story
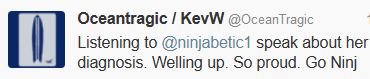
I only got involved with the Diabetes Online Community after a friend spoke about Laura’s Ninjabetic support group (read this) being in the news. We’ve spoken on Twitter so many times that Laura seems like a member of the family and I know her story so well.
Laura, Mark and I had tweeted earlier in the week about Laura’s speech: she didn’t know what to say. She suggested the three of us do a flash mob but luckily Mark and I turned it around and suggested she just spoke about herself, about her diagnosis, about her salvation from the dark days of ignoring diabetes care.
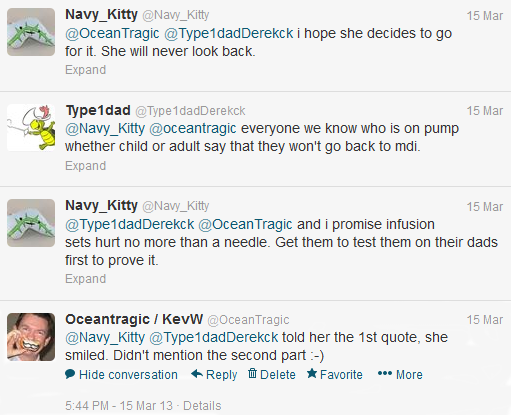
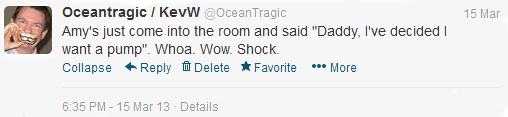
She spoke from the heart about her diagnosis, a story I could relate to so well, a story I knew off by heart. I was quite moved, more than I’ll admit to for sure. My tweet sums it up:
Speed dating starts
We all sat around the 7 tables, there was six on ours including me, Amy, Laura (@ninjabetic1) and Mark (@thedteam2) who’d travelled all the way from Swindon, plus two other guys from the Portsmouth area.
Each of the 7 professional people/teams switched from table to table to table in true speed dating fashion, having 8 minutes each.
In those 8 minutes we had to get through multiple questions from our side and theirs. This event wasn’t just about patients getting answers it was also about professionals finding out what patients require, so that they can improve their service.
All in all it worked very, very well, it was just that 8 minutes wasn’t enough, we could have done with about 30 minutes each, but that just wouldn’t be realistic.
Meeting Derek, refreshments and quiz time
At 11:15ish we broke for refreshments which gave me a chance to chat with my friend from work. Whilst talking 76 year old Derek Bockett said hello and we had a nice chat. I recognised him from last year’s JDRF Walk To Cure which we’d done. He’s an amazing chap, 76 years young, full of life, fit as a fiddle and has had type 1 diabetes for 61 years! He told us to keep active and make sure we kept ourselves well. What a great advocate for diabetes.
Amy came up and asked me to fill-in the carbohydrate counting quiz: she’d done it and wanted to increase our chances of winning the prize. I didn’t bother.
Talk by Dr Cranston
Back in the room and Dr Cranston (Consultant Diabetologist – and more importantly Laura’s pump consultant) gave a great presentation about what’s on the horizon for type 1 diabetes, current stuff, future stuff and some quite complex stuff. I enjoyed the talk even if some of it flew right over my head.
I really admire Doctors who give talks like this. As a geek I know how hard it is to get things across in a language which is understood by the layman, without comprising what you need to say and the points you need to get across. Dr Cranston did this extremely well.
The quiz result
It was time for the carbohydrate counting quiz result.
Who had guessed the right amount of carbs for a Sunday Roast and a Spag Bol? Not on the same plate you realise, there was two plates 🙂
“The roast was 50g”. Amy whispered an emphatic “Yes!”
“The spag bol was 90g”. Amy wispered “darn, I said 100g”.
“And the winner is….Amy Winchcombe”
I let out a “Yesssssss!”
The problem was the the prize was a bottle of champagne and Amy was 12 and it wasn’t good form for a healthcare professional to be giving alcohol to a 12 year old. I said that that’s the standard age to start drinking in Portsmouth but (luckily) no-one heard me.
The champagne was given to Laura, sat next to Amy, who put it on the table.
Yay, we’d (erm I mean Amy had) won some champagne.
I’m so proud that in a room full of diabetics many of whom have counted carbs for years that Amy’s knowledge proved the best. Well done Amy.
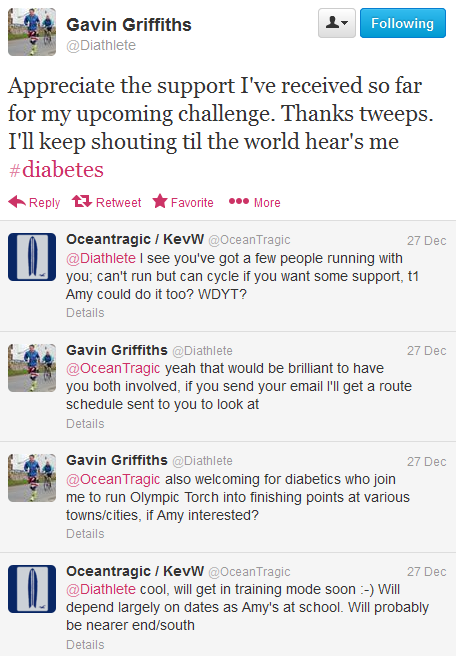



 Gav’s GBR30/30 Challenge poster
Gav’s GBR30/30 Challenge poster

 He has type 1 diabetes himself, as have relatives of his, but not his siblings and he spoke about them, getting diagnosed and using multiple blood samples of theirs in his research to discover why he got it but they didn’t.
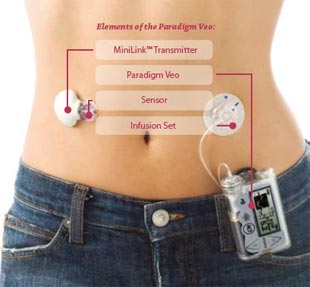
He has type 1 diabetes himself, as have relatives of his, but not his siblings and he spoke about them, getting diagnosed and using multiple blood samples of theirs in his research to discover why he got it but they didn’t. Animas Vibe insulin pumps
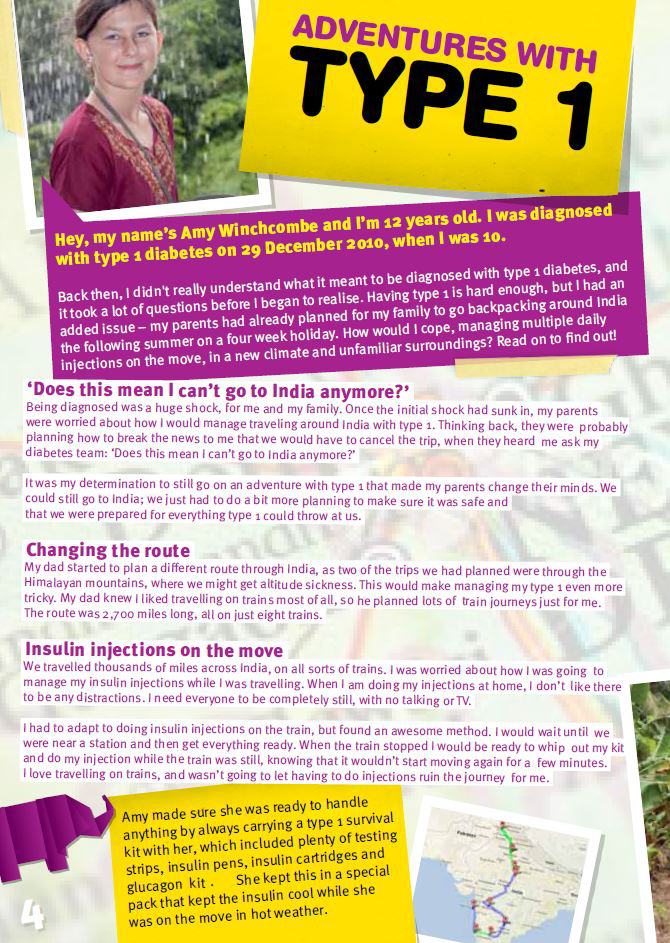
Animas Vibe insulin pumps Amy (in pink) on the front cover of the JDRF T1 Kids magazine
Amy (in pink) on the front cover of the JDRF T1 Kids magazine
 Dr Iain Cranston let’s us know about future improvements
Dr Iain Cranston let’s us know about future improvements

 Animas Vibe pumps
Animas Vibe pumps Animas Inset II infusion sets in multiple colours
Animas Inset II infusion sets in multiple colours
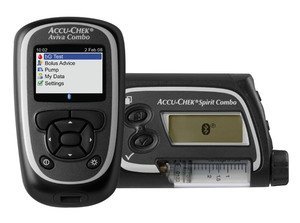 Roche Accu-chek Combo pump and meter
Roche Accu-chek Combo pump and meter Accu-chek Aviva Combo meter, almost identical to the Aviva Expert
Accu-chek Aviva Combo meter, almost identical to the Aviva Expert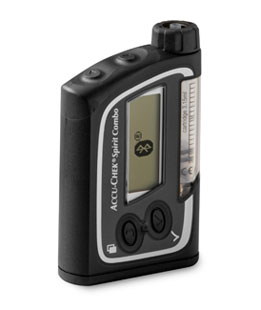 The Accu-chek Spirit Combo pump
The Accu-chek Spirit Combo pump Rapid-d
Rapid-d Flexlink
Flexlink Tenderlink
Tenderlink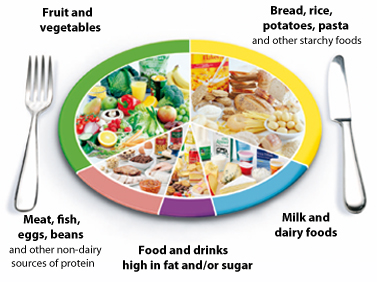 The NHS Eatwell plate.
The NHS Eatwell plate.  There’s many rungs on the ladder towards the pump
There’s many rungs on the ladder towards the pump