“I should have been there to inspire you”
I was playing a Paul Weller’s Heavy Soul album in the evening after Amy’s clinic in December 2012, the one where she fainted.
My favourite tune from that album came on and it made me think, take a listen whilst you read the rest of this article
httpv://www.youtube.com/watch?v=VWls8s-G8m8&list=ALBTKoXRg38BDyREOUtVcf5edcCo8stOXC&autoplay=1
Nice song, shame about the lyrics – well kind of
Mr Weller’s written a beautiful song there but actually the lyrics point towards someone who’s failed someone else at some point in their life. Someone who knows now, when it’s too late, that they should have put something in place to help someone else.
Jane and I aren’t perfect parents by any stretch and we will fail at some bits but we can’t afford for it to be Amy’s diabetes management; we won’t let that happen.
“I should have been there to inspire you…”
I love that line and when I hear it it makes me think, “yes, I too want to inspire”.
It struck me that we need to inspire Amy to create a positive attitude around diabetes and not a destructive one; an attitude which gets on and deals with what needs to be dealt with; an attitude which makes her want to take care of herself; an attitude which makes her want to stay fit; an attitude which keeps her from diabulimia through the next impressionable years.
More importantly I never want to have to say the words in the song when it was too late, when something bad had happened, because that something bad could well be life threatening or disabling.
“…not paint your world a cold, cold blue”
The aptness of the lyric was not lost on me.
Blue, being the colour of the international diabetes symbol.
Blue, being the colour associated with sadness/depression.
Starting with fitness
Trying to get or stay fit can be hard work; it’s always seemed too much like hard work for me, but I loved playing sports even if I wasn’t that good at them.
Amy’s not particularly sporty, she’s not a member of any clubs, but she loves trying new things and so it began. We stepped up visits to the Leisure Centre and I introduced Amy to the game of Squash, something I played every week back in my 20s (yes, yes, it was a long time ago!).
Amy loved/loves Squash and in the first few weeks we ended up playing it twice a week. We’ve missed a few weeks here and there, interspersing it with Badminton and generally having great fun doing it.
I should add that this has been made so much easier but our local leisure centre operator DC Leisure, whose off-peak price for a court when a child is playing is only £1.95 for 40 minutes, instead of £6.90. Well done DC Leisure, you’ve made it so much easier to teach my kid a sport and get them interested.
Starting with attitude
I wanted Amy to know she wasn’t alone, being a kid with type 1 diabetes. She already knew that Dad spent far too long on Twitter talking to adult people with type 1 diabetes and we’d taken part in #GBDOC’s first ever Kid Tweetchat, but honestly she’s too young for Twitter at the moment.
I’d read about the JDRF T1 Youth Ambassadors programme and got Amy to sign up, to become part of something, to join a collective that intends to help get the facts about diabetes right.
She needed no persuasion and signed up immediately.
More to follow on this further down the page.
Starting with fitness and attitude
At the December clinic our Endocrinologist/Doctor and I were discussing use of Twitter and the DOC when she said that she had heard a talk from an inspiring young type 1 runner from London who went by the name of, I stopped her and said “Gavin? Griffiths?”.
(Sorry Doc, oops, won’t do it again.)
She was clearly very impressed with Gavin’s attitude to diabetes and how he dealt with and managed it.
Gavin (@diathlete) and I have followed each other on Twitter for a while now and I was well aware of his amazing plans for running from John O’Groats to Land’s End during April and May 2013, in an challenge known as the GBR3030.
I approached Gavin and asked if would be okay if Amy and I cycle next to him for one of the 30 mile legs of his journey; he seemed pleased at the idea.
I brokered the idea with Amy who gave an immediate “yes”.
If one ounce of Gavin’s never-let-diabetes-stop-you attitude rubs off on Amy I’ll be a happy man.
We currently plan to cycle the Bodmin to St Agnes route on the 25th May, the penultimate day of Gavin’s challenge, with Amy raising money for DiabetesUK and JDRF.
To donate please use the main donation page for GBR3030.
Helping with education too
Amy’s already written a few very well received articles for this blog, so well received that her diagnosis article was the second most read page, only just behind my World Diabetes Day post.
I needed her to write the final article for our series about travelling in India with type 1 diabetes which she did, making her remember the things that she did were already amazing to some, making her realise she’s achieved things that some people will never achieve making her remember how diabetes did not control her on that trip.
That article quickly became the top article on the blog and I couldn’t be a prouder parent.
JDRF seem impressed with that article too and if all goes well it might feature in one of the next T1 Kids magazines.
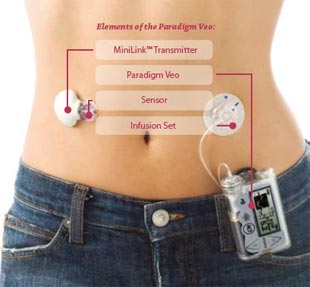
What’s this got to do with getting an insulin pump?
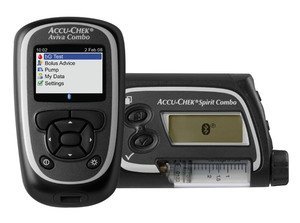
Well, the final bit of the jigsaw for me was that I already knew that in general pumps are pretty good news.
I wanted Amy to know about them but this was going to be hard, although not quite as hard as I thought.
Hopefully you’ve already read the blog articles about the 15th March so you’ll know what progress was made during and after the clinic.
I truly believe that some of the stuff we’ve started this year has had a good effect on Amy’s attitude toward diabetes. Her interest in management has increased and her knowledge too.
Without all of this I don’t think she’d be on the waiting list for an insulin pump.
And finally, my New Year’s resolution
At a party on New Year’s Eve, midnight came and everyone hugged, chinked glasses and kissed. Friends wish each other good times, but Amy was nowhere in sight.
When she appeared we hugged, kissed and wished each other Happy New Year and she asked “Dad, what’s your New Year’s resolution?”
I decided not to tell her the only thing on my mind: “to inspire you with your diabetes management, to set you up for a healthy future, to get you a pump if you want one, all in 12 months.”
This may well be the first New Year’s resolution I’ve ever kept.
Thanks for reading.