I met Lucy and her family about a year ago, at an event organised by the local (South Hampshire area) families support group, Seahawks. We’ve spoken quite a bit, through highs, through lows and one day I offered her the chance to tell her story.
Have you already read part 1, Night-crawler to Day-walker or part 2, Night-crawler to Nightscouter?
Here’s part three of a three part story.

Paige and me enjoying a coffee soon after diagnosis
A BIG THANK YOU
When Sienna first got diagnosed all our family and friends grouped together and helped us gain our new normal, living life just a bit differently. Friends arranging their working lives, arranging their own children’s bedrooms to accommodate our three children, to arrange the washing of their school clothes for the next day at school all whilst Sienna’s close family gathered around and had their own training on T1.
Our friends joked saying it was like a play group with all the children playing together, but that they were all well behaved. I think our heads were obviously not in the right place to remember to thank everyone for their own efforts. We really do have some amazing and very loving friends, they really have stood by our sides through the worst and have shared some awesome highs. So to all the people that have stood by, watched over us, helped out in anyway and have taken the time to learn and ask about T1 we really are truly thankful to them.
Eighteen months on and now with Nightscout and Dexcom in tow we have taken our normal and smashed it. We have found caring for Sienna less stressful, don’t get me wrong for us we still work hard on her D everyday it’s just a little bit easier and her HbA1c is now at a health 7.5.
A big sister’s knowledge
It’s a Friday night sleep over for Paige with a friend having sweets, treats and films. I had the girls in one room with mattresses on the floor and as we do every night we go up and check Sienna’s levels.
Paige’s friend is a lovely sweet girl with a heart of gold was very inquisitive that evening asking if Sienna’s finger clicker hurt her and would it hurt her. With that I wound the needle around and down then offered it to her “you can try it if you want” she shied away and said she couldn’t do it, with that Paige nicked it off her and said “here I’ll show you how to do it”.
This girl from day one has amazed me with her knowledge of T1 and taken a keen interest in caring for Sienna as a big sister. She knew how to click her sisters finger and get the reading as well as carb count and enter the carbs in her meter. She knew the diabetes book like the back of her hand and got involved in doing a 2 minute discussion at school talking about and spreading the word on type 1 for a competition. Such a chatterbox I think she said she talked for six minutes, I giggled when she told me. Massive well done.
(Off track slightly but who’s not going to big up their child at any given minute especially at a time like this.)
That sinking feeling
Paige clicked her finger and read out that her bloods were 31.6mmol.
31.6mmol!
 She shocked herself so I went on to say that because she had been eating sweets that she must go was her hands. Right at that moment my heart sank slightly and every part of me right there so desperately wanted the next reading to be a hell of a lot lower. Some part of me was trying to justify such a high reading, maybe she had way too much to eat.
She shocked herself so I went on to say that because she had been eating sweets that she must go was her hands. Right at that moment my heart sank slightly and every part of me right there so desperately wanted the next reading to be a hell of a lot lower. Some part of me was trying to justify such a high reading, maybe she had way too much to eat.
I asked them what they had had.
They had shared one small packet of jellies and half packet of toffee popcorn so there was no way in hell it should have been that high. I love candy floss and have eaten a whole packet (Obviously, I’m not sharing that, so I’m going to eat the whole bag) and could probably eat a lot more and still my sugars wouldn’t be that high after.
She came back after washing her hand and said to her friend that sugar on her hands would give a false reading. My heart melting again because she has just retained so much information but I knew deep down that our journey would start again only this time Paige had a very unwanted friend onboard.
Heart in my mouth
Again she clicked and with my heart in my mouth I prayed and hoped to God.
Please, please don’t let it be higher I said to myself. The meter beeped and read HI.
My heart skipped numerous beats and inside I sank.
We all remember the first time we went through a diagnosis! Yep, that feeling. Paige’s face dropped but she looked to me and basically wanted reassurance that maybe she didn’t wash her hands properly. “Yes definitely and No I’m not worried” I said. Going to see her dad I explained the situation. He said exactly what had whizzed in and out of my mind in seconds before and that was maybe she had eaten too much too quick. The realisation of that statement meant that he was trying to justify to the reason why, Love this man to bits but this time I was not a paranoid mum. I quickly got online and told my T1 family about the situation and asked for guidance.
Thank you for all the replies back offering help. Within seconds twenty or so responses came back saying to go with her and wash her hands and to click a toe and reassured me that I should take her straight to hospital, to check ketones and to give plenty to drink etc.
Paige had been weeing a lot that evening not that I noticed as she’s old enough to take herself to the loo as well coming down for more drinks.
In total disbelief
It was only when I sat in total disbelief on the sofa that all the pieces started fitting together. I decided to go with her and wash both her and my hands. We clicked again, this was now the 3rd click and the meter beeped again to read a HI for the second time. I did ketones to see how poorly she was but they were 0.1.
I knew then that if we went to hospital she would be seeing the diabetes team that day without fail but how could I actually turn around to her and say “Yes you have type 1 diabetes” but at the same time I didn’t want to lie to her. When Sienna was diagnosed she was very poorly but this diagnosis was at the opposite end of the scale and Paige was a lot older. Her friend came downstairs whilst I rang the NHS to get more advice and even the nurse said as she’s only just finished eating that her sugars would be high. Sorry but this was rubbish I thought to myself.
One more test and hour later and she was still HI, I explained that we would be going to hospital and that she would have to have a test to see how poorly she was but at the same time not saying that she definitely had D. We left daddy snoring in bed and woke my 11 year old son up to keep said friend company, they had been friends since pre-school so she wouldn’t feel left out so to speak.
 Sienna supports her sister in hospital
Sienna supports her sister in hospitalA journey forgotten
We gathered our things and drove off to the hospital and I’m really sorry but I can not remember our conversations on her possibly having T1.
On arrival to the hospital it did take forever for her to be seen but once she was she had to have another clicker. Now for some people like us with young one’s you do think of their poor fingers and how sore they get after 3,360 or so clickers and the broken skin. A very emotional downfall to T1D as well as the cannula insertions on delicate skin and the amount of time we have to hurt our children to insert a needle. The constant numbers running around our heads, we now had double the work to do, double the dose of insulin to deal with as Paige is older her insulin doses were a lot higher, Double the pain of watching them go through this and not being able to take it away from them, treating both Hi’s and Lo’s throughout day and night was doubled a mammoth task that we now faced. But we DID IT and we will continue to do it for as long as it takes because we have to.
I have always said and will continue to say that as parent of T1D we all take an emotional battering everyday but put it all to the back of our heads and it only comes to the surface when talking or writing about this condition.
A journey shared
We shared Paige’s journey throughout her stay at hospital with our T1 family and we gained a few more friends along the way, we had been promoted to the families with two T1’s. Paige made the doctors and nurses jaw drop with how much she knew and how brave she had been doing her 1st injection and now that we have settled into some sort of normality she is still brave as all T1’s are. Watching Sienna in hospital being so supportive, so loving and empathetic to Paige was admirable for all to see. Sienna was offering Paige her hand to hold whilst she watched her do her injection and stroking her knee telling her how brave she was. All these things she remembered Paige did and still does with her.
They will forever and always have T1D to deal with but nothing can smash the bond of being a sister and we will not let anything stand in their way.
So to all you Supermums, Dads, Grandma’s, Aunties, Uncles, Brothers and Sisters you can do it, as a friend once told me you are braver than you were yesterday, stronger than you think and smarter than you seem.
Xx


 Sienna wearing her first Dexcom G4 sensor
Sienna wearing her first Dexcom G4 sensor Sienna has an awful hypo
Sienna has an awful hypo



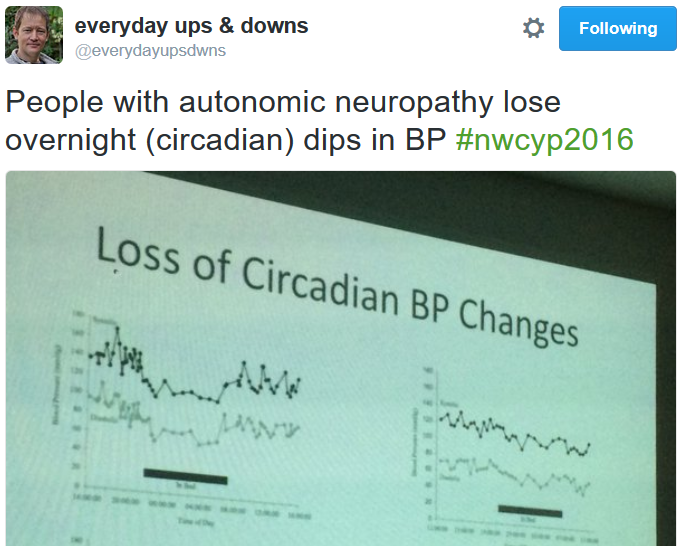 Dr Weston’s presentation started with Autonomic Neuropathy and almost lost me within minutes; I feared today’s presentations might be too much for my little brain to understand but actually it was fascincating, and scary, but mainly fascinating.
Dr Weston’s presentation started with Autonomic Neuropathy and almost lost me within minutes; I feared today’s presentations might be too much for my little brain to understand but actually it was fascincating, and scary, but mainly fascinating.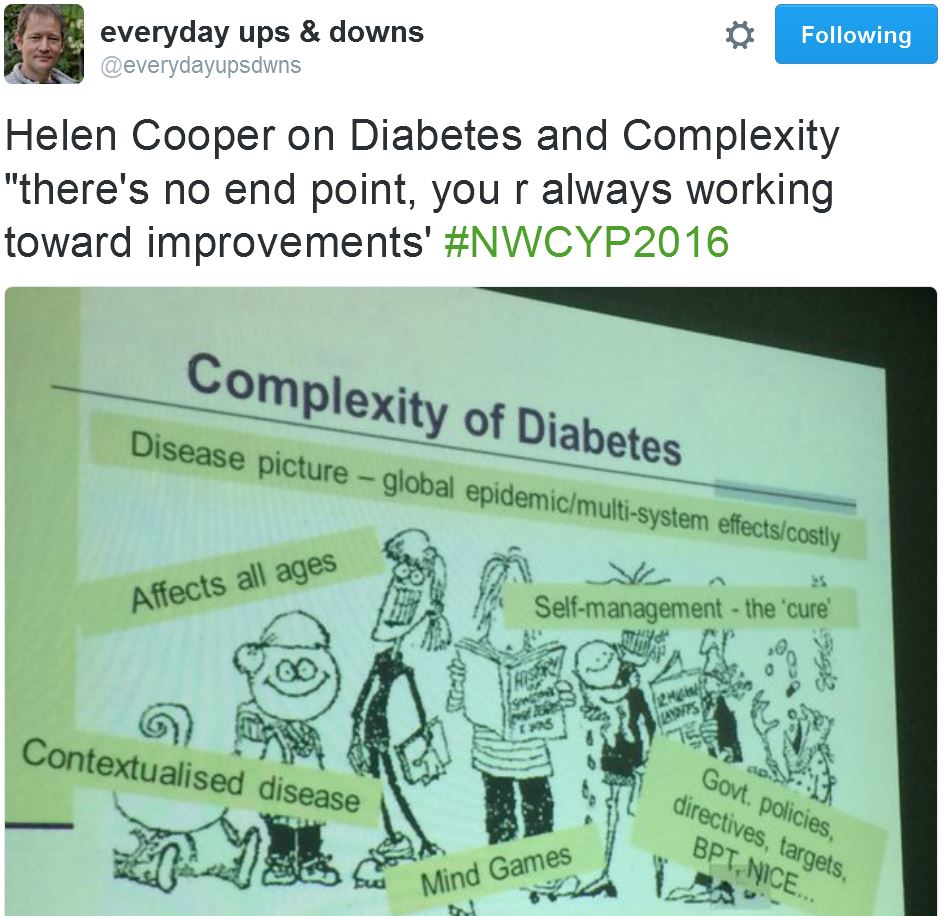 Not only leading in her field, Professor Cooper is proof that having Type 1 need not stop anyone and she’s proved this during the 50 years since being diagnosed. I find it wonderful being in the company of people with such experience and each one (Derek, Lis, Pat and now Helen) has a great and happy outlook.
Not only leading in her field, Professor Cooper is proof that having Type 1 need not stop anyone and she’s proved this during the 50 years since being diagnosed. I find it wonderful being in the company of people with such experience and each one (Derek, Lis, Pat and now Helen) has a great and happy outlook. Dr Agwu presented about Toddlers with Type 1, something I’ve always been grateful we didn’t need to deal with: people often say they don’t know how families like ours cope, well I don’t know how families with toddlers cope.
Dr Agwu presented about Toddlers with Type 1, something I’ve always been grateful we didn’t need to deal with: people often say they don’t know how families like ours cope, well I don’t know how families with toddlers cope. Mike is a natural presenter, eloquent, factual, meaningful messages and (sadly for me) too blooming funny: how on earth was I going to have the funniest presentation after his?
Mike is a natural presenter, eloquent, factual, meaningful messages and (sadly for me) too blooming funny: how on earth was I going to have the funniest presentation after his?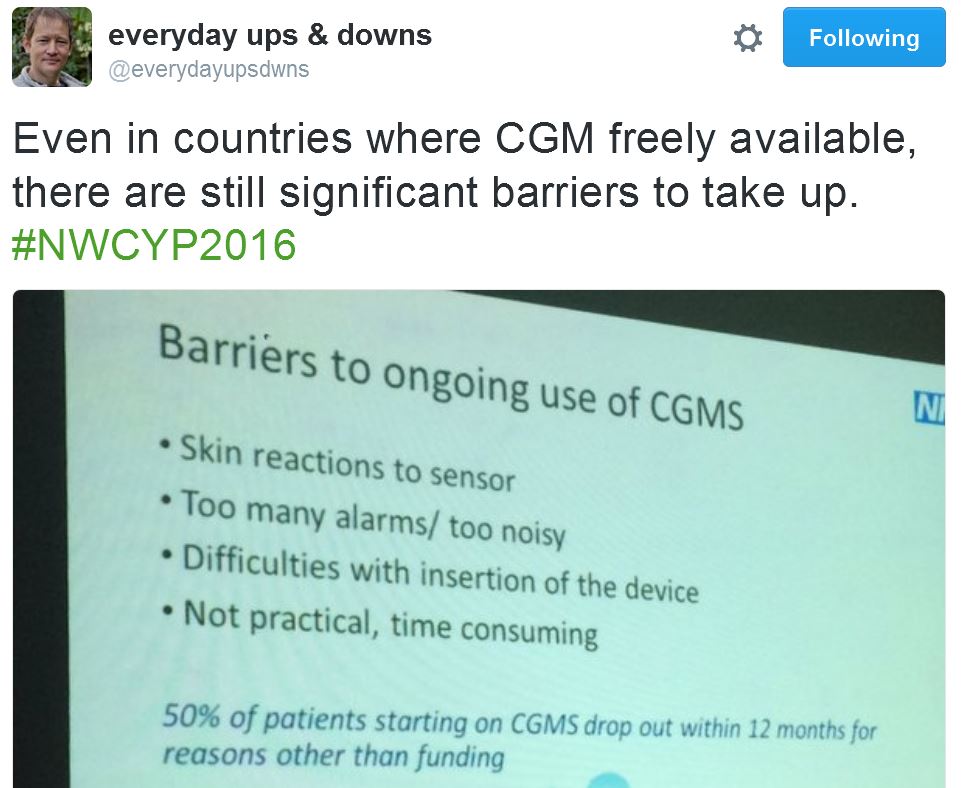 Dr Krone gave a great talk about the benefits of CGM and gave some real life examples of people who thought their diabetes management was excellent yet spent most of every night in a very long hypo.
Dr Krone gave a great talk about the benefits of CGM and gave some real life examples of people who thought their diabetes management was excellent yet spent most of every night in a very long hypo. After the tea break it was my turn.
After the tea break it was my turn. Due to my running well over time Helen had little time left, I felt guilty.
Due to my running well over time Helen had little time left, I felt guilty.


 Was it really four years ago that Jane took Amy to the Doctors to find out what was wrong? Four years since the Doctor took that simple blood test and called us within minutes to tell us to go to hospital? Four years since my daughter found her
Was it really four years ago that Jane took Amy to the Doctors to find out what was wrong? Four years since the Doctor took that simple blood test and called us within minutes to tell us to go to hospital? Four years since my daughter found her 

 Announcement of new blog, November 2012
Announcement of new blog, November 2012 Excerpt by Dr Kar, Roche Reach magazine, Winter 2013
Excerpt by Dr Kar, Roche Reach magazine, Winter 2013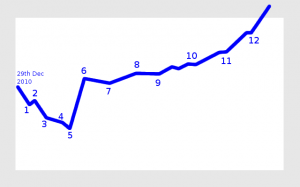 My view of our diabetes journey
My view of our diabetes journey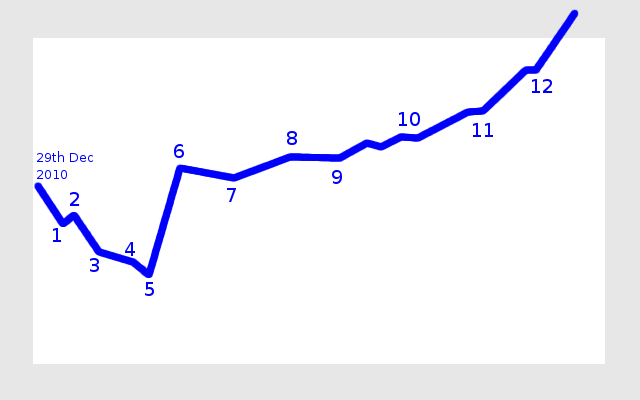
 Download my “How social media helps us with Type 1 Diabetes” leaflet
Download my “How social media helps us with Type 1 Diabetes” leaflet




