
Amy and her new insulin pump and her new DiabeTees iPump t-shirt
A busy (sinful) 24 hours
Since waking up yesterday morning, Jane, Amy and myself have had a great 24 hours, almost a day of celebration of the new pump, a day of treats and especially a day of saying ‘what the heck, just have it’. On reflection this may not have been the best policy on only day 2 of a pump, it just snowballed.
I’ll hold my hands up then and say that on the face of it today we’ve been pretty irresponsible, we’ve let our daughter got all out and eat want she wanted. I’ve made sure we ended in places where she’d say ‘ooh, can I have that?’ so we could let her.
It wasn’t meant to be like this.
A couple of weeks ago we chatted about the impending first 24 hours on the pump and said that we would be good, eating only normal food and stuff that we could easily calculate the accurate carb value for. This was especially to make the carbs/insulin matching accurate so that we knew that glucose fluctuations would be mainly down to Amy’s basal insulin, which the pump delivers every few minutes. This in turn would help our DSN (diabetes specialist nurse) make adjustments to Amy’s basal profile, something that is crucial to the pump being a success.
Early rush for clinic
Amy’s 3 monthly clinic appointment had been booked for yesterday since the last one in March, on the 15th.
That was the one where Amy first saw a pump and later had her epiphany moment and said “I want a pump”.
So our ‘time to pump’ was one clinic, or a little over 3 months. (15th March to June 20th). It could have been quicker if I hadn’t been researching pumps for so long.
Clinic was at 10am, we only just made it.
It was strange being back there the day after the time before, the only times this has happened before for Amy was when she was diagnosed and before that, when she was born. She didn’t remember the first time for some reason.
Whilst I have no experience of other clinics can I just say that I blinking love this one: everyone is part of one team, a team which encourages, helps and listens.
The dreaded hbA1c check/result
For those of you who don’t know the hbA1c is a blood check which in layman’s terms tells the Dr how ‘good’ you’ve been for the last 3 months. It’s a little more complicated than that, but that’s the gist. Many argue that hbA1c is not a good test as you can have a ‘good’ result whilst living a life of hypos and hypers, with blood sugars rollercoasting, whilst a ‘bad’ result could be achieved with very little fluctuation. Many, including me, would argue that the latter (‘bad’) is a better thing to strive for. Dave Sowerby’s article delves into the HbA1c check in more detail.
Amy was generally 7.3 but in December rocketed to 8.3, in March she was back down to 8.0.
I feared for today’s result as she’d been high on average for weeks. We’d done nothing about this as she was going on a pump and it seemed little point changing things about.
The result came in….
8.2
Phew! I was amazed it wasn’t a little higher.
First up: DSN
Our DSN and Dietician attended the first part, looking over the last 21 hours (since going live on pump) log book information. This felt strange, we were only talking about 21 hours, not the normal three months.
They were pleased with the progress made already, amazed at how well Amy looked and felt about the pump, applauded the BG values and corrective doses.
Whilst the DSN said not to bother two-hourly testing through last night, I suggested that we were happy to do it if it meant her basal might be easier to get right.
She agreed and said she’d give us a call – in her own time – sometime later this morning.
Second up: the Doctor
Some people dread the first few minutes of an appointment with their Endocrinologist, but not us, for one simple reason: she always starts with ‘how are you Amy’. She always talks direct to Amy, she leads with questions about her wellbeing and doesn’t lead with ‘your hbA1c result showed that…’.
I love this approach.
We spoke mainly about the pump, how it was going, what it felt like, did the cannula hurt and things like that.
I asked how she found the training day the day before, trying to elicit a response about the Animas pump. I wanted to try and see if there was any issue with us wanting the Animas Vibe and daring to challenge the de-facto standard issue of Medtronic or Roche.
“I like that pump, I think more people may get that one here. What were the reasons you really wanted it?”
This was excellent news, there was no problem about us wanting the Vibe and great news that the Doctor liked it. I went through the many, many reasons we chose Animas over the others.
We offered to come in to do demos for other parents/children who were looking at pumps.
Costa: an easy place for diabetics
It was 11:30am, Jane and I were knackered after a lack of sleep last night. I needed caffeine, so we hit Costa in the hospital grounds.
“Have what you like Amy”
“Really? O.M.G. I’m having that” as she pointed to the Mango and Passion Fruit Ice Cooler.
I should explain that normally Amy would just have water, it’s 0g carbs, or at best a Diet Coke, never something she’d need to bolus for as that would mean another injection. Now it doesn’t, just a couple of button clicks.
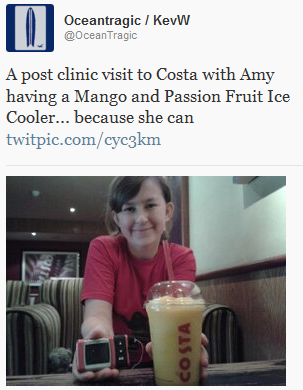
Jane asked how many carbs and the Barista asked where were sitting and that he’d be one minute.
He turned up with a huge book which he said listed absolutely everything they sold. And it did.
The drink was a massive 55g of carbohydrates, so Amy bolused 4.25 units of insulin for it. What was nice was that she didn’t do a blood test for it, just used the ‘ezBG’ feature to match the insulin to the carbs consumed.
She loved that drink, she loved the feeling of having things she’d denied herself for years.
Retail therapy
We spent the day with some retail therapy, visits to fast food places (which we never normally do) and even succumbed to buying a box of Krispy Kreme doughnuts for film-watching time later that evening.
Amy was ecstatic at the new world opening up to her.
We did have a discussion about everything returning to normal today.
Later that evening I reflected on the way forward:
Two hourly testing results
We’ve got to test Amy’s blood glucose levels every two hours for the 48 hours after having pump. This is something everyone going on a pump seems to do, although for many they have to do it for a week.
Amy’s levels have been:
Time, BG mmols, correction dose
06:00, 3.6, 9g carbs (mis-calculated carbs for 3 dextro, thought it was 5g each, it’s only 3g! Discovered mistake 30 minutes later)
08:00, 5.7
09:00, 4.9
10:00, 5.9
11:00, didn’t test but had 55g smoothie drink, 4.25u insulin
12:00, we were travelling so we forgot/missed this check
13:00, 7.4, lunchtime, eating huge 105g carbs so had 8.05u insulin
14:30, 4.2, 9g carbs, Amy felt hypo so even though technically wasn’t she had 9g to make her feel better. It worked.
15:00, 3.6, 15g carbs, clearly 30 minutes she was dropping quickly
16:00, 6.5
18:00, 14.2, 2.55u insulin, clearly the 9g+15g Dextro tabs earlier had caught up with her
19:00, 11.7, dinner of 56g so took 6.03u insulin – 4.3u insulin for the food, 1.73u insulin for the correction to bring her levels into range
20:00, 6.8, 40g carbs & 3.05u insulin – post-dinner treat doughnut
22:00, 4.1, 24g carbs for a milkshake, no insulin suggested
00:00, 14.7, 2.35u insulin
02:00, 8.8
04:00, 9.1
06:00, 8.0
Considering what a ‘treat’ day it’s been those figures are amazing.
#Winning
 Monday’s topic:Let’s kick off Diabetes Blog Week by talking about the diabetes causes and issues that really get us fired up.
Monday’s topic:Let’s kick off Diabetes Blog Week by talking about the diabetes causes and issues that really get us fired up. 

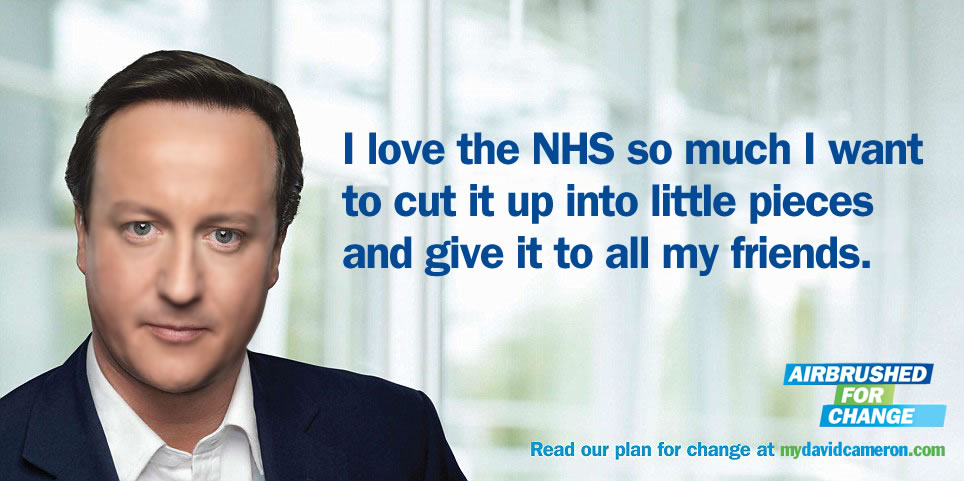 image from http://mydavidcameron.com/
image from http://mydavidcameron.com/ Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt
 Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt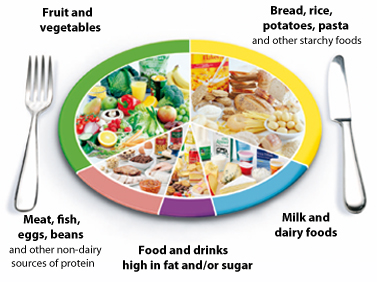 The NHS Eatwell plate.
The NHS Eatwell plate. 