The start of a whirlwind long weekend of diabetes events was an event organised by our clinic which jointly covers the Royal Hampshire County Hospital and Basingstoke Hospital, and their surrounding areas.
There was one last year and I found it really good, an opportunity to speak with our consultant outside of clinic walls, to mingle with other parents and grill the reps.
Truth be told I was rather nervous about attending this event.
The last time we saw the team was this fateful day back in January and my anger at the apparent complete disregard for our wishes almost saw us transfer elsewhere. So this would be the first time we met since that clinic. How would it go, would I lose it or could we still be ‘friends’?
I decided to put that last clinic down as a bad job, a mistake, a misunderstanding and walked into the room as if that clinic had never happened. And I’m so glad I did. Things appear to be back to normal although we’ll not know for sure until the next clinic.
These events are great for networking and we’d agreed to meet several people there; Steve and Becky; Matt, Sonal and their daughter who adores Amy. I bumped into Claire who runs the Basingstoke PWD group and I suddenly remembered I’m meant to be talking about Social Media and Nightscout there soon so I went over to discuss it. (*writes date in diary before he forgets*). Amy had made a little gift for Matt’s daughter who was thrilled.
The room filled with families and many of us left to listening to the Tech talk. Matt and I haad hoped to present Nightscout as part of this talk but its lack of clinical trials meant we were denied. Shame really as I think the parents needed to hear it, it would have been far more appropriate than talking about Smart Insulin etc.. But then again, there seemed to be so many families who nothing of this stuff. One person even asked if there was any truth that Reiki could help, something I consider as helpful to Type 1 as slapping, although hopefully less harmful.
Matt and I had joked that I’d ask a question after the session, that question being ‘Matt, what’s your daughter’s glucose level right now?’ and looking at his Pebble he’d reply ‘x.xx mmmol/l, how about Amy’s?’ at which point I’d look at my watch. We never did, I bottled it. It could have been funny though right?
The next session was about Transition and Amy and Jane sat in for that. I was gasping for a drink so headed out only to bump into fellow DiabetesDad and cyclist Gavin. Gavin asked if I could chat with him about Nightscout for 640g and I creased up as Matt (the 640g Nightscout solution provider) was a metre away. “Matt, meet Gavin” I mentally said Sorry to Sonal for given her husband even more support to do, although I’m pretty sure Gavin will figure it all out.
I never ventured back into the Transition talk and it’s probabably a good thing as Jane told me that apparently at the first transition clinic they see the kid first and then the parents and child together afterwards. So why on earth did they not do that with us? I just may have exploded if I’d been in there.
I had a chat to Emma, our pump rep, quizzing her on the rumours of Animas’s next pump name, release date and features. She’s good though and gave nothing away, thinking obviously that no-one in the community knows about the 2017 release date of the pump which like Medtronic’s 670g will feature a hypo and hyper minimiser. I already knew that this new pump will use Dexcom G5 as its base, we’d prefer G4 of course with its 4x longer lasting transmitter, but G5 will be awesome in this pump.
It had been a great night, lots of interactivity, lots of chats, lots of meetups and more importantly I’d not glared at the team.



 I’ve taken part in many of the weekly (Wednesday night at 9pm) #GBDOC tweet chats since they started a couple of years ago, I enjoy them and generally get a lot out of them. A couple of weeks ago I got a message from Paul (@t1hba1c) who hosts the #GBDOC tweetchats who asked whether I’d like to host a tweetchat about bring up children with diabetes. I was initially reluctant: why would anyone want to listen to or answer my questions; there’s many more parents who with their eloquence could host a great tweetchat.
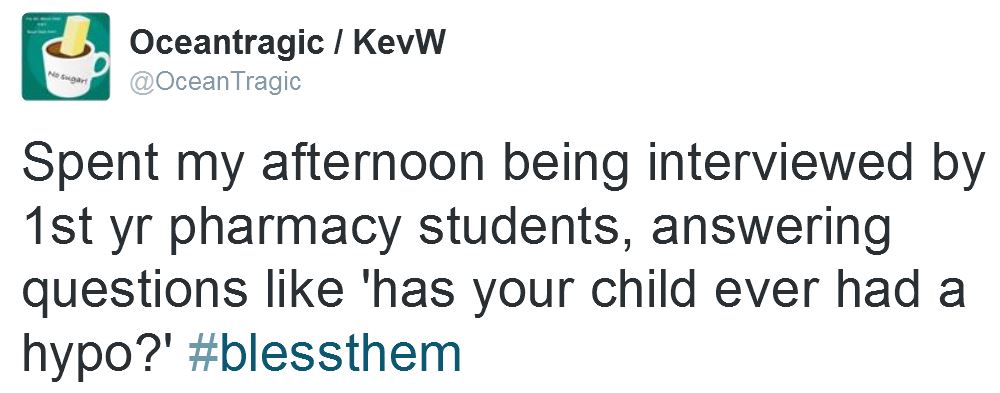
I’ve taken part in many of the weekly (Wednesday night at 9pm) #GBDOC tweet chats since they started a couple of years ago, I enjoy them and generally get a lot out of them. A couple of weeks ago I got a message from Paul (@t1hba1c) who hosts the #GBDOC tweetchats who asked whether I’d like to host a tweetchat about bring up children with diabetes. I was initially reluctant: why would anyone want to listen to or answer my questions; there’s many more parents who with their eloquence could host a great tweetchat. Back in April Dr Kar (@parthaskar) from the neighbouring QA hospital asked if Amy would be up for helping him out at a conference he was going to, the National Paediatric Diabetes Team Meeting hosted by Lilly in Birmingham. I guessed she wouldn’t, it’s not her thing, but I asked and she said ‘Yes’, her thoughts of helping Partha outweighing her fear of public speaking.
Back in April Dr Kar (@parthaskar) from the neighbouring QA hospital asked if Amy would be up for helping him out at a conference he was going to, the National Paediatric Diabetes Team Meeting hosted by Lilly in Birmingham. I guessed she wouldn’t, it’s not her thing, but I asked and she said ‘Yes’, her thoughts of helping Partha outweighing her fear of public speaking.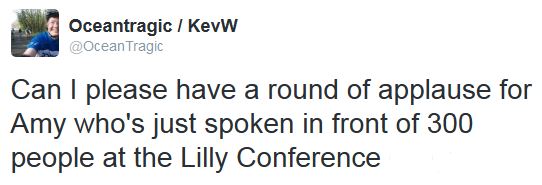


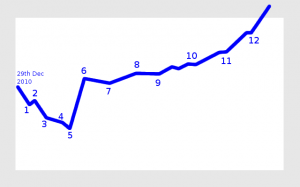 My view of our diabetes journey
My view of our diabetes journey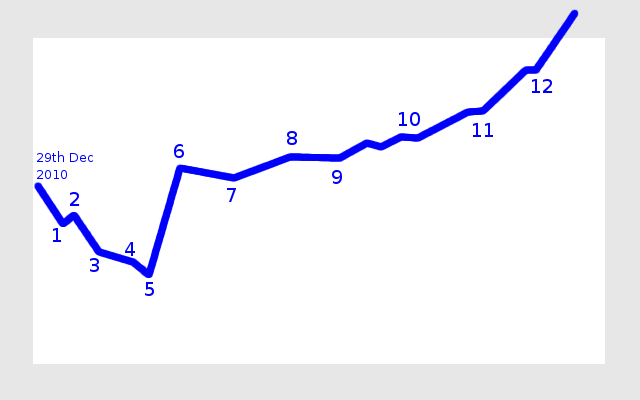
 Dr Iain Cranston let’s us know about future improvements
Dr Iain Cranston let’s us know about future improvements

 Animas Vibe pumps
Animas Vibe pumps Animas Inset II infusion sets in multiple colours
Animas Inset II infusion sets in multiple colours There’s many rungs on the ladder towards the pump
There’s many rungs on the ladder towards the pump


