Amy, aged 10, at the caves in Ellora
In late July 2011, exactly 7 months after Amy was diagnosed with type 1 diabetes, we backpacked around India for four weeks, in a trip we called Monsoon Meandering.
This is the last post in the 14 article series about that trip and its planning and how type 1 diabetes played a part.
The previous posts are full of facts and viewpoints but this one is the most important, it’s the story from Amy about what she remembers about the trip and adjustments she had to make.
Hey, the name’s Amy.
I’m 12 and I was diagnosed with type 1 diabetes on 29th December 2010.
My family and I were already planning to go to India the following summer and we were going to go to Ladakh which is in the Himalayas. After I was diagnosed my parents quickly started to wonder whether we should go to India or not. Through his research Dad had found out that getting altitude sickness was a real possibility on the two road trips through the mountains and he wasn’t happy about dealing with that at the same time as diabetes, both of which we knew nothing about. So it was decided, we would not be going to India that year. Thinking back now, they were probably trying to figure out how to break the news, when they heard me say to the doctor “Does this mean I can’t go to India any more?“. It was this that changed their minds. We were going to go to India (even if we went somewhere different) and nothing was going to stop us.
Changing the trip plan
Whilst thinking of an alternative trip my Dad tried to think specifically what I liked the most about India; it was trains. He decided that we should go on lots of them, just for me.
Altogether we travelled around 2700 miles on just 8 trains and the trip was organised all by ourselves! No help whatsoever from travel agents or such. We saw monuments, holy places, tombs, caves, palaces, trains, beaches, cities and we even went to a waterpark – we were the only ones there! How cool is that!? All of that for a whole month.

The beautiful Golden Temple (Harmandir Sahib) in Amritsar
Flying, excitement, worries about injections
I have been to India once before – before diabetes – and I loved going on the plane so I was really excited about going on it again, but I was worried about the injections and the food. Before it came to mealtime we told the staff that I was type 1 diabetic and they went and found an apple for my pudding. Also they gave me my food first in case I had to count carbohydrates (which at that point I didn’t because I was still in my honeymoon period but it was still very thoughtful of them). When it came to injection time I was worried and didn’t know how we would do it, but my mum, who was sitting next to me, set it up and did it in my arm and the best bit was I didn’t even have to get out of my seat!

Henna powder on sale at a market
I love India’s trains
Trains are exciting because I barely use them in England and there’s very few sleeper trains, which I love. A sleeper train – clue’s in the title – is a train which has padded benches for you to sit on during the day, which then turn into beds for during the night. India has so many of these because the distances are so great, some trains go for three whole days from start to finish. We travelled thousands of miles across India by train using upper class, middle class and lower class trains. The poshest train was from the capital city (Delhi) to Amritsar (the hottest of the places we went). We had padded, reclining seats and were served meals by waiters in traditional Indian uniform, it was the fastest train we took.

On one our many trains, in a side-berth in class 2A
Overcoming fears of injecting on the trains
I don’t like any distractions when I do my injections at my house so I have to have the light on full, have everyone completely still, have no talking or T.V and no cats moving in the room. So when I did the injections on the trains I had to adapt but everything went well as we came up with an awesome method. First we would wait until we were near a station, then when the train stopped I would have my injection ready to whip out and do. If I did it as soon as the train stopped, then I would be sure that it wouldn’t start to move whilst I was in. But I love trains, and I wasn’t about to let diabetes ruin them for me.

Relaxing in our 4 berth compartment in two-tier air-con class (2A)
Weird ceremonies in Amritsar
Whilst at Amritsar we saw the stunning Golden Temple and we witnessed the weirdest ceremony ever (video) – where they close the border gates between Pakistan and India. There were men dressed in Indian army suits with stupid fans sticking up on top of their turban! There were people running up and down the road and when they got to the Pakistan border, they waved the Indian flag in their faces. As the border closed the soldiers goose stepped up to the gate and almost stuck their tongues out at the Pakastani soldiers, however it was all in good humour…or was it?

Some silly walking in the border closing ceremony between Pakistan and India.
Here’s the video
Loving the Homestay adventure
One of the many adventures that we had in India was going to live in a Homestay. This is where (clue’s in the title again) you stay in one of the local’s homes. We knew that we were going to the Homestay and that they’d be poor, so we decided to bring our old clothes and school uniforms. We gave it to them and although they were girls clothes, and our hosts only had boys, they took them gratefully. We also gave them a frisbee and a bat & ball which they loved and they taught me a new game that I can still remember now. Coming back to the diabetes side of it, I did my injections after my meals because I decided three days in to the one month trip that I didn’t like India food any more. What a fail. It turned out that it was just one thing – paneer, a type of cheese they use in curries – which I’d gone off.

Eating our first home cooked meal – rice, dal, aloo chat and roti – at the homestay

Our host, Malti, prepares our pakora breakfast over a wood fired stove

Our host, Malti, waits for the pakoras to cook, in the room where she eats, sleeps, cooks and lives
httpv://www.youtube.com/watch?v=8L-9KBGnIl4
Jamming in Hampi
Another place we went was Hampi which looks as though a giant has scattered some pebbles (what we would call boulders) in totally random places. Hampi is a small village with lots of huge rocks randomly placed around the landscape. It has a many temples, a market, a river and plenty of places to stay. It was so beautiful.
I met a music man, he came from far away,
now I can play (what can you play?)
I play the kololu.
Kolo-kolo Kololu Kololu Kololu Kolo-Kolo Kololu Kolo Kololu.
The music man was called Gali and he taught me to play the Kololu (think of a flute then turn the buttons into holes and make it wood) for free. I decided to buy it but we didn’t have the money with us right then so he said take it and pay me back tomorrow which was really nice of him as he didn’t really know us.

Mummy, Emilia and me walking to The Mango Tree through a banana plantation
The world’s best Mango Tree
There is only one word that can describe The Mango Tree; magical. The Mango Tree is a cafe/restaurant where you can sit outside to eat and watch the river and all the wild life around it. The Mango Tree was a little walk away from where we were staying but it was worth it. We had to walk through a banana plantation and when we got there I had a Banana Paratha and a Banana Milkshake. We sat on the straw mats on the floor and waited for our food and then I spotted a Kingfisher in front of the river!

Mummy and me enjoying the view at The Mango Tree restaurant in Hampi

My banana parantha was so yummy and was served on a banana leaf
httpv://www.youtube.com/watch?v=MYtgqw8IHY4
Lakshmi the Elephant takes a river bath
Talking of animals, one day in Hampi my family and I went down to the river to see Lakshmi the Elephant having a wash. It was funny because they asked if anyone wanted to be blessed by Lakshmi and my mum was determined to, but when she saw that actually it meant she would have to go in the river and get a full soaking of water from Lakshmi, she decided not to.
As I said earlier, I have been to India twice, and last time I went, we went safari-ing and we saw many animals including an Indian Rock Python and a Tiger chasing a Wild Boar!

Lakshmi walks past me on the way down the ghats (steps) to the river

Lakshmi lays down in the river whilst being washed by her Mahouts, who are the people who take care of the elephant
httpv://www.youtube.com/watch?v=pf24ZMD5K1Y
Getting my first tattoo
One of the many things that India is famous for is Henna. Henna is an ink which is used to draw a pattern onto your arms or legs. It stains your arms or legs until two weeks later when it eventually fades away. Generally it is used for women on special occasions such as their wedding day however when I was out in India I got my Henna done within the last week so I could show my friends. I had it done on both my arms and I bought some Henna powder so I could make some more at home, and I still have it after one and a half years.
Here’s a video of me buying henna/blocks at the market in Orchha

Me testing the henna colours & blocks in Orccha’s colourful market

Henna pattern on my arm
Thank you for reading about my adventures, I hope my story makes you realise that diabetes doesn’t have to stop you doing things you want to.
Amy.

Our family in the Gopi Restaurant in Hampi

 She’d done similar stuff before, she’d spoken in front of 200 HCPs twice before but then the answers she gave were very short. She’d presented Nightscout and WeAreNotWaiting alongside me to Directors at JDRF and Diabetes UK, and to the team at Oxford. DPC2017 was different, as she stood there – alongside my friend Philippa and Dr Hussain – she answered Dr Hussain’s questions, elaborating on them with anecdotes and telling stories about school life, German exchange trips and the difference between two holidays in India, one on MDI, the next one using an insulin pump.
She’d done similar stuff before, she’d spoken in front of 200 HCPs twice before but then the answers she gave were very short. She’d presented Nightscout and WeAreNotWaiting alongside me to Directors at JDRF and Diabetes UK, and to the team at Oxford. DPC2017 was different, as she stood there – alongside my friend Philippa and Dr Hussain – she answered Dr Hussain’s questions, elaborating on them with anecdotes and telling stories about school life, German exchange trips and the difference between two holidays in India, one on MDI, the next one using an insulin pump. 





 Amy and her new insulin pump and her new DiabeTees iPump t-shirt
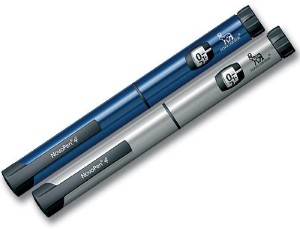
Amy and her new insulin pump and her new DiabeTees iPump t-shirt Animas Vibe insulin pumps
Animas Vibe insulin pumps Amy, aged 10, at the caves in Ellora
Amy, aged 10, at the caves in Ellora