 Back at the end of July Amy went on a trial of the Dana RS insulin pump, a trial which was due to last four weeks, two of which we were on holiday in France.
Back at the end of July Amy went on a trial of the Dana RS insulin pump, a trial which was due to last four weeks, two of which we were on holiday in France.
The trial was successful, Amy has asked for the pump and whilst it’s not cut-and-dry her Consultant is very hopeful that her request will be approved.
Controlling the pump via the AnyDana-A 2.0 app
We had delayed starting the trial as we wanted to test the new Android app, Anydana-A 2.0, which can be used to control the pump totally, being able to do anything on the app you can do on the pump. At the the start of the trial (30th July) the app wasn’t released but three days later as we travelled through France we got the call from Tom, our DanaRS and Advanced Therapeutics representative, to say the app was live.
Within minutes the app was downloaded, installed and was talking to the pump.
Simple.
Wait, what, you used the app in preference to AndroidAPS?
Yep.
The important part of this trial was to trial the pump, its cannulas and general day-to-day wear, tear and usage. We don’t need to check whether AndroidAPS works for Amy because it’s based on OpenAPS and that works very well for her, plus other users have millions of hours of experience – not each, jointly – of OpenAPS and AndroidAPS.
That works, no question.
So then, the pump?
The pump, being one of the smallest and lightest currently available in the UK, was comfortable to wear, coming with a whole range of clips, holders and things which we’ve really no idea what they’d be used for.
All pumps have similar features and Dana RS seems to have all the ones Amy requires, plus she found the menus easy to use on the pump, then again that was only for the first few days until the app arrived.
Amy found the reservoir changes easy and the only downside is possibly that filling the reservoir is a little fiddlier than she’s used to BUT a major advantage is that she only has to change reservoirs every six days. Hmm, should I write that on a public page? Six days? She says she’d rather spend a few seconds fiddling with “that screw” (see below) if it means she can change reservoir less often, with its insulin wasting, looking-for-bubbles-time-consuming nature.
Big downside though: her trial pump was grey not pink. Euw, eh?
And the cannulas?
 The rather funky cannulas caught Amy’s attention immediately, with their 360 degree spinniness and the ability to disconnect rather than rip-out during an inevitable door handle moment.
The rather funky cannulas caught Amy’s attention immediately, with their 360 degree spinniness and the ability to disconnect rather than rip-out during an inevitable door handle moment.
The cannulas worked well but did leave a raised doughnut shaped mark and we didn’t think about trying anything to stop that happening. After the trial finished we realised we should have contacted Tom as he had many suggestions to try, and even let Amy continue using the pump for a further two weeks until she ran out of cannulas. During that time she used Cavilon for the first time and that seemed to help.
So then, the app?
In the first week the app had a few display issues but the developers were really on it, responding to feedback and rolling out minor tweaks every day it seemed, updates which really slowed down as they ironed out the issues.
Using it was easy and I found myself saying to Amy at each meal time “have you bolused?” as I was used to seeing her pull out a pump, but that’s a thing of the past with this app.
Here’s a video Amy did to show to do a simple bolus, a combo/multi bolus and how to change a basal rate:
So then, “that screw”?

A couple of people who used a Dana R – the RS’s predecessor – as part of Dr Hovorka’s trials have mentioned about “that screw”, which is part of the pump/reservoir, putting out negative comments which others mention as the reason not to go for a Dana pump. The problem for me as that the originators don’t make a big thing of it, others do, why? Anyway, the Dana pumps work differently and has a screw which clips into the reservoir – see this video for more info. Honestly this process takes seconds, if that, way less that other parts of the refill process.
AndroidAPS: wait, what, you used it?
For the actual trial I didn’t even look at AndroidAPS for Amy, but after Tom suggested extending the trial I just went for it.
Within an hour or so the software was all installed properly on her phone and she was offline closed-looping.
And. It. Is. Brilliant.
It’s so easy to set up, it is offline from the word go and most importantly Amy can configure it all herself because it’s on her phone. She would technically have been able to configure her OpenAPS too but that would involve more faff than she was interested in doing.
Take a look at this time-lapse of 5 hours of AndroidAPS in 60 seconds. Keep an eye on the temporary basals shown in blue, especially the area the vertical dashed-line goes through.




 Amy’s new Camoflage Pink SPIbelt
Amy’s new Camoflage Pink SPIbelt


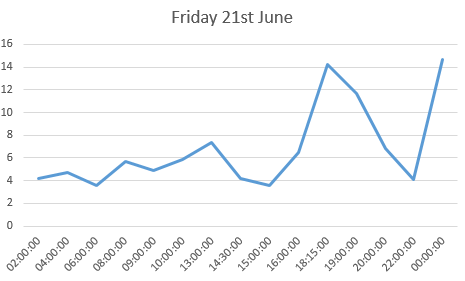
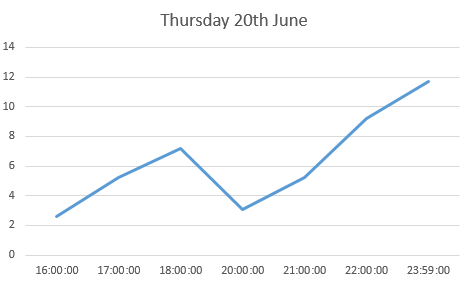
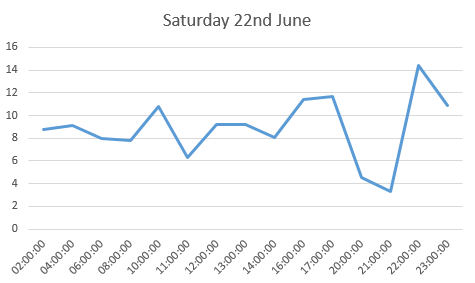
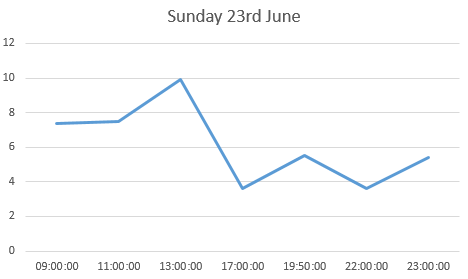
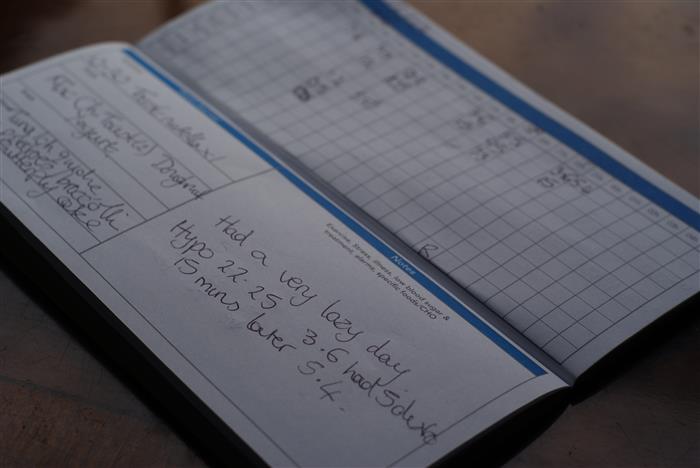 the log book page for 23rd June
the log book page for 23rd June Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt
 Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt Amy awoke excited at what the day would bring.
Amy awoke excited at what the day would bring.

 Animas Vibe insulin pumps
Animas Vibe insulin pumps Animas Vibe pumps
Animas Vibe pumps Animas Inset II infusion sets in multiple colours
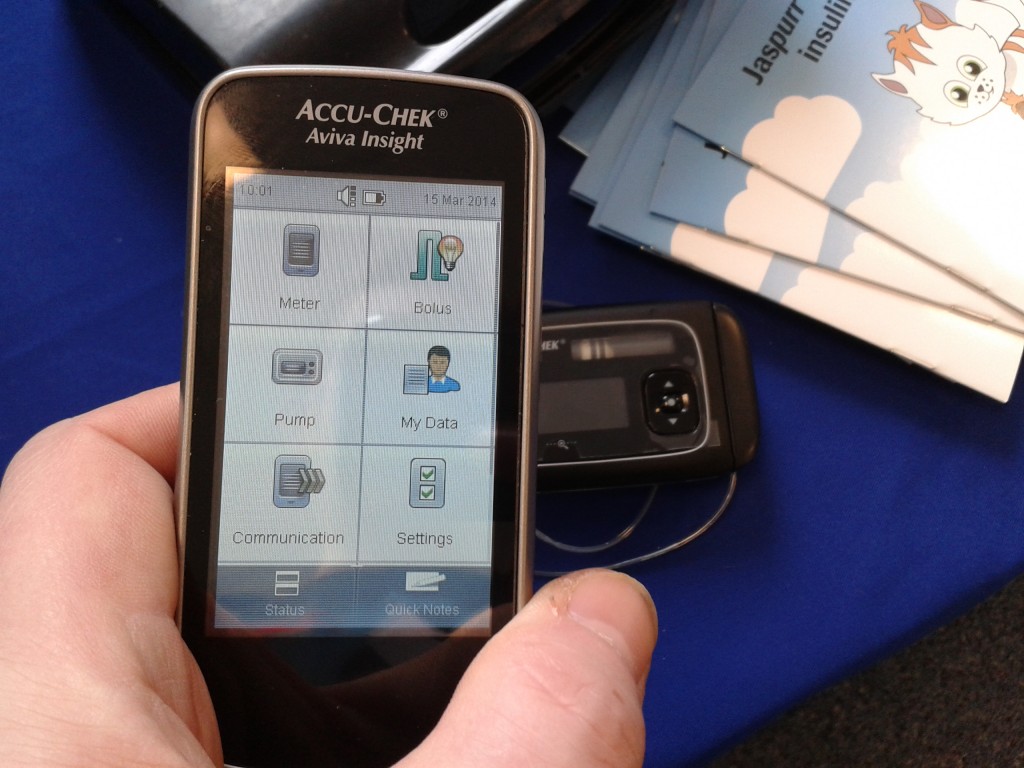
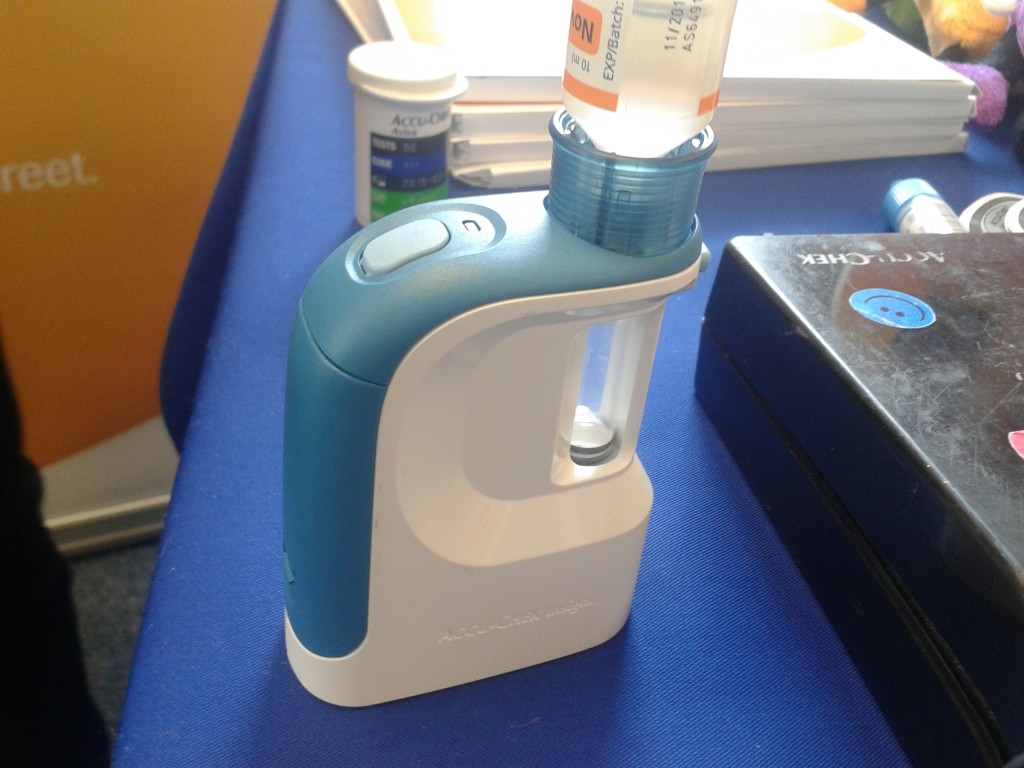
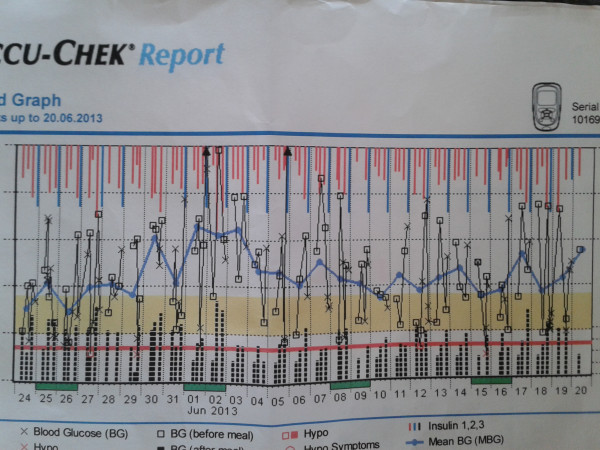
Animas Inset II infusion sets in multiple colours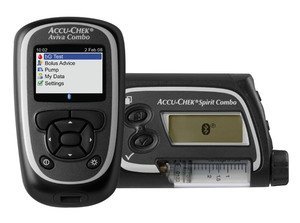 Roche Accu-chek Combo pump and meter
Roche Accu-chek Combo pump and meter Accu-chek Aviva Combo meter, almost identical to the Aviva Expert
Accu-chek Aviva Combo meter, almost identical to the Aviva Expert The Accu-chek Spirit Combo pump
The Accu-chek Spirit Combo pump Rapid-d
Rapid-d Flexlink
Flexlink Tenderlink
Tenderlink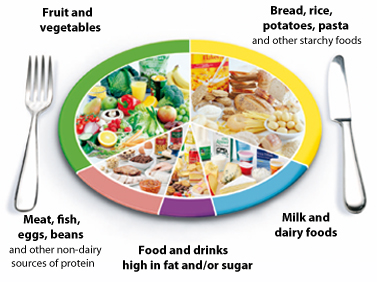 The NHS Eatwell plate.
The NHS Eatwell plate.