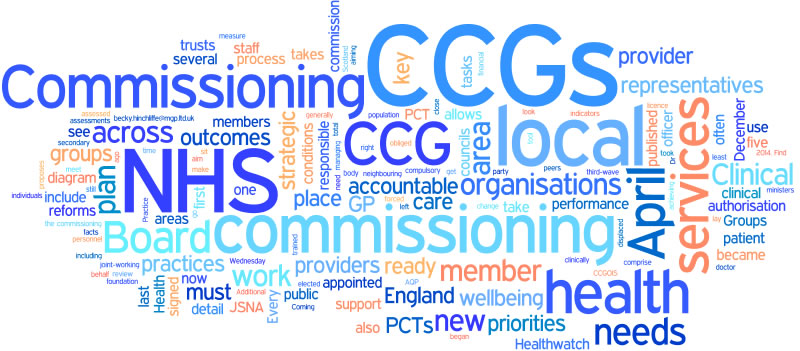
It all started by chance
On Tuesday 17th September at the end of my first ever Diabetes UK Winchester Support Group meeting I was chatting with Lucy & Daisy from Diabetes UK and a lady came to sit down next to me to chat – I wondered what I’d said wrong 🙂 That lady was Beverley Meeson and turns out she’s the Associate Director in Long Term Conditions at West Hampshire CCG. A prominent figure in an organisation we already owe a lot to and here she was asking little old me for information. We spoke about Amy’s new pump and she asked it was one of the new ones with integrated CGM (Continuous Glucose Monitoring). “Yes” I laughed “but it’s irrelevant as the CCG won’t pay for them.” I couldn’t help myself. Oops.
Seizing opportunities
True to my word I emailed Beverley the very next day with details of our journey to getting a pump and pointed her towards my many articles on the subject.
Beverley forwarded my details to Janet Hutchings who was organising a patient focus group for Type 1 Diabetes adult care, who emailed to see if I could come along to a meeting, which was happening the following Monday.
It was going to be a struggle to take the afternoon off at such short notice, was it really worth it and could I really be bothered?
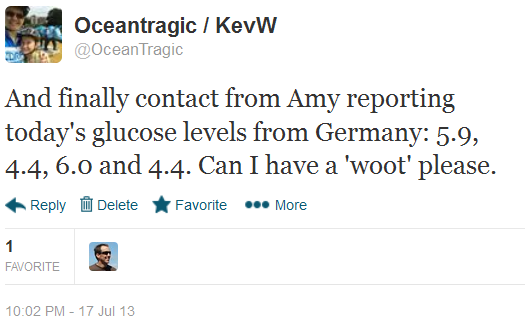
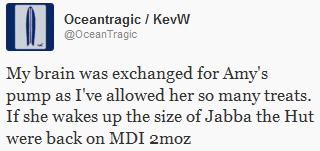
A tweet out brought replies which convinced me to go
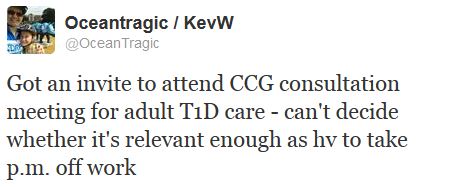
That was it then, I was going, if my boss would agree.
The agenda
Janet had said that she wanted an informal meeting so that it would facilitate more open discussion but at the same time wanted to discuss certain topics, so set a rough agenda:
Welcome and introductions; How did you hear about this meeting?; Your current experiences of the service (positives/negatives); What would enable you to manage your diabetes better?; What would a quality service be for you?; How could we use innovation and technology to improve services?
Woah, did you see that last one? I’d best save my voice for that bit!
Introductions by everyone there
It was quite a small affair but I think it was better this way as it gave us all a chance to speak. If there’d been too many no one would have had a chance.
The meeting was chaired by Janet of the CCG.
Patient number one was Dave, who said he was confused whether he was Type 1 or Type 2 as people tell him different things. I took this to mean that he was an insulin-dependant Type 2 as Dave seems to only see his local GP and nurses. Or perhaps he’d been missed off the lists at the hospital?
Patient number two was Andrea, who has had Type 1 for 40 (I think) years and attends a mixture of two local hospitals, one of which is our one.
Patient number three was Martin, who was diagnosed in the 80s whilst in his late 20s. He attends a different hospital and some of the same places as Dave.
“Patient” number four was me, an interloper who’s got nothing to do with adult care for people with Type 1 Diabetes.
How did you hear about this meeting?
Janet had a big list of people she’d contacted to get the message out there about the meeting.
Not one of us had heard about it from the official channels and had generally found out by chance or coincidence, something Janet felt she needed to work on next time.
Your current experiences of the service (positives/negatives)
Once everyone had gone through their list of of positives and negatives of the current system one thing became clear: all our experiences are completely different and could be labelled as the usual ‘postcode lottery’. Given that we all fall under the same CCG this seems strange and hopefully something that can resolved with some guidance.
One person spoke about how they are forced to go and have an HbA1c done at their GP’s, one month after being done at the hospital. If they don’t go they don’t get their prescription filled and therefore don’t get any insulin or test strips. I suggested to the CCG that this was a pointless time-wasting inefficient box-ticking exercise, given that a GP is not likely to suggest altering ratios or start discussing Super Bolus-ing or any some such.
Interestingly for me, I didn’t think I’d have too much to say here but it seems paediatric experiences are similar to those for adults.
What would enable you to manage your diabetes better?
Test strips and knowledgeable GPs seemed to be the consensus.
With test strips the postcode-lottery rears its head again, or more to the point it’s the subjectiveness of the GP that drives the issue. Andrea pointed out the history of test strips being refused, something that Janet paid close attention to. Part of the problem seems GP’s confusion between the two main types of diabetes. Again clear guidance and education from the CCG to the GPs should save the day.
The other three key points were education, education and education but with it a big caveat: we all agreed that courses organised and run by the hospitals were needed and we spoke about the DAFNE style courses and how beneficial they’ve been to those who attend. The caveat (raised by us patients) was that patients should not sit back and expect to be told everything, that patients should be encouraged to be proactive in their condition. We felt that the hospitals could signpost new patients to other resources, something they don’t seem to readily do at the moment.
I spoke about instant HbA1c tests and how some people had to organise a blood test weeks before their appointment. Martin didn’t understand what I meant as he didn’t even know this was possible as it seems it’s only done like this in paediatrics. But why? There’s a machine sitting there in the hospital in Winchester, why not use it!? I suggested that this would make like easier for people and at not a huge cost. Janet wrote this down to investigate further.
What would a quality service be for you?
We spoke about the 15 Healthcare Essentials; about care in hospitals; about GP’s understanding of the different types of diabetes; about access to DSNs.
I – who came prepared 🙂 – spoke about Portsmouth CCG’s Super Six model and ask whether the CCG had looked into it – they had and will investigate further.
Andrea and I spoke about the patient focus innovation that was the Portsmouth “Sweetmeet”, something both Andrea and I attended.
(I started to wonder whether I should not mention Dr Kar’s name again in case it started to wind up the CCG 🙂 )
I spoke about transition from paediatrics to adult care and may have inadvertently mention Dr Kar’s name again, along with his article Changing services can actually be fun.
How could we use innovation and technology to improve services?
Janet asked about technology improvements and how they could help patients.
I cleared my throat.
This was my time to talk.
With reference back to our discussion earlier about patients taking partial responsibility for their own education I started talking about my recently created and released leaflet ‘How social media helps us with Type 1 Diabetes‘. Luckily I’d printed a few out which I handed out for people to read.
I spoke about virtual clinics for people who have trouble getting to the hospital, access to hospital information, standards of care, social media groups run by the hospitals and so on.
I may have gone over my allotted time 🙂 Oops!
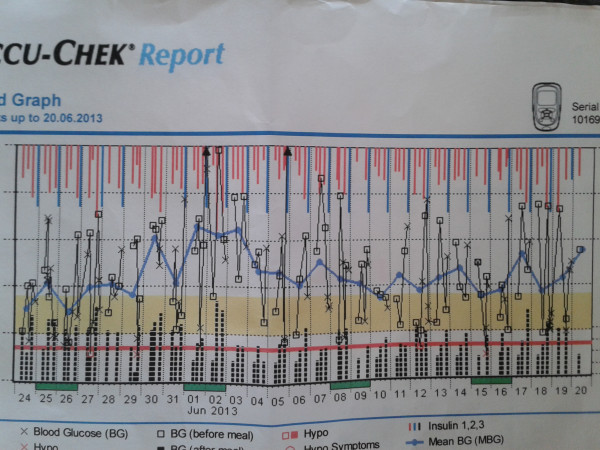
On top of this I spoke about my use of Diasend, how the hospitals can access the information and how this could help patients.
And finally
I’m so glad I attended this meeting and would like to thank both Janet and Beverley for allowing me, a mere interloper, to attend.
I think it’s great the CCG are encouraging patient focus and collaboration and look forward to working with them in the future.
Thanks.


 An HbA1c checking machine
An HbA1c checking machine





 Amy’s new Camoflage Pink SPIbelt
Amy’s new Camoflage Pink SPIbelt


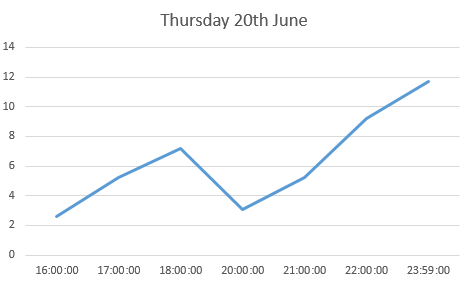
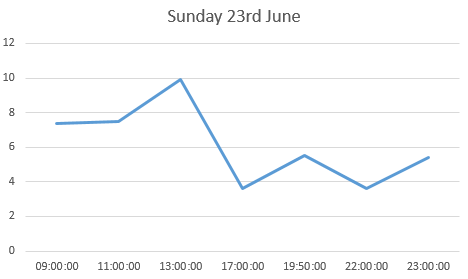
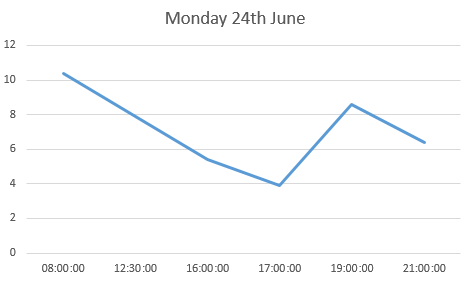
 the log book page for 23rd June
the log book page for 23rd June Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt
 Amy and her new insulin pump and her new DiabeTees iPump t-shirt
Amy and her new insulin pump and her new DiabeTees iPump t-shirt Amy awoke excited at what the day would bring.
Amy awoke excited at what the day would bring.

 Animas Vibe insulin pumps
Animas Vibe insulin pumps