 Back in April Dr Kar (@parthaskar) from the neighbouring QA hospital asked if Amy would be up for helping him out at a conference he was going to, the National Paediatric Diabetes Team Meeting hosted by Lilly in Birmingham. I guessed she wouldn’t, it’s not her thing, but I asked and she said ‘Yes’, her thoughts of helping Partha outweighing her fear of public speaking.
Back in April Dr Kar (@parthaskar) from the neighbouring QA hospital asked if Amy would be up for helping him out at a conference he was going to, the National Paediatric Diabetes Team Meeting hosted by Lilly in Birmingham. I guessed she wouldn’t, it’s not her thing, but I asked and she said ‘Yes’, her thoughts of helping Partha outweighing her fear of public speaking.
Part of the excitement was getting chauffeured to Birmingham in a shiny Mercedes but he was due at 11:30am and should have been here 15 minutes ago. Our house is notoriously hard to find and it turns out he didn’t have my mobile number. Finally I found him by walking around the area and we were off. I quick call to Nicki at Lilly and we found out Amy was on at 14:45, our ETA 14:30, perfect. That was until the roadblock north of Oxford which saw us divert towards London. ETA 14:50, not so perfect. Nicki said don’t worry though.
Rushing into the hotel Nicki met us and Amy got miked up, alongside 19 year old Rebecca who goes to QA, but where was Partha: stuck at Oxford. The chair, Dr Fiona Campbell, padded out for a bit but it was clear Partha wasn’t going to get here in time and the show must go on. Easy for adults to adapt to but not so easy for a 13 year old with a fear of public speaking. Fiona took control and Amy and Rebecca took to the stage.
The idea of the slot was to be a chat show, with Partha calmly asking Amy and Rebecca questions about their care, what they like, what they don’t and what would be the ideal service for them. Amy knew these questions and we discussed in the car how she’d like to respond, trying to make the experience as easy for her as possible. Trouble is Fiona didn’t know these questions, nor the interviewees, but I must say that she winged it incredibly well.
Amy looked nervous on the sofa sat next to Rebecca but then I saw she was also sat next to Alex Silverstein, someone whom I follow on Twitter and we’re friends on Facebook but our paths had never yet crossed. I felt better, Alex would take care of her I thought, although of course he didn’t know it was Amy sat next to him.
With the first question asked Rebecca gave a great long answer, before Fiona asked Amy who then got a bit tongue tied. More and more questions asked and Amy opened up giving great answers with the information she knew about. She was asked about talking to the GP about diabetes and said she never had and wouldn’t as she’d talk to her diabetes team. Fiona asked why Amy wouldn’t think about going to the GP and Amy answered exactly the same way I would: if it’s diabetes related we’ll go to the people who are the specialists.
Questions were asked about Skype consultations, preferred types of wards for any hospital admissions (general young persons’ ward or specialist diabetes) and whether they’d prefer letters being addressed to them or their parents. Letters? No thanks, these are young people, they want emails, or (as suggested by Fiona) text messages. They were asked if they ever saw a post-clinic letter, they hadn’t. I felt like stepping in and saying that yes we get a letter, two months after clinic, a letter which informs us of our insulin-pump-wearing child’s basal-bolus units and ratios but nothing about her pump’s basal profile or insulin:carb ratios. That letter goes straight in the bin.
With the show over Amy’s first DSN Debbie came over to see us. She had no clue we’d be there and took a while to recognise it was Amy on stage, but she was so proud, remembering that 10 year old who she’d helped through her first injection. I was bowled over to see Debbie again and similarly to meet Alex after all these years. I shared text messages with DSN Sarah who works in Southampton but couldn’t see where she was in the room. One of our DSNs was at the conference but we never managed to see each other. But that wasn’t too much of a surprise in a room of 300 or so.
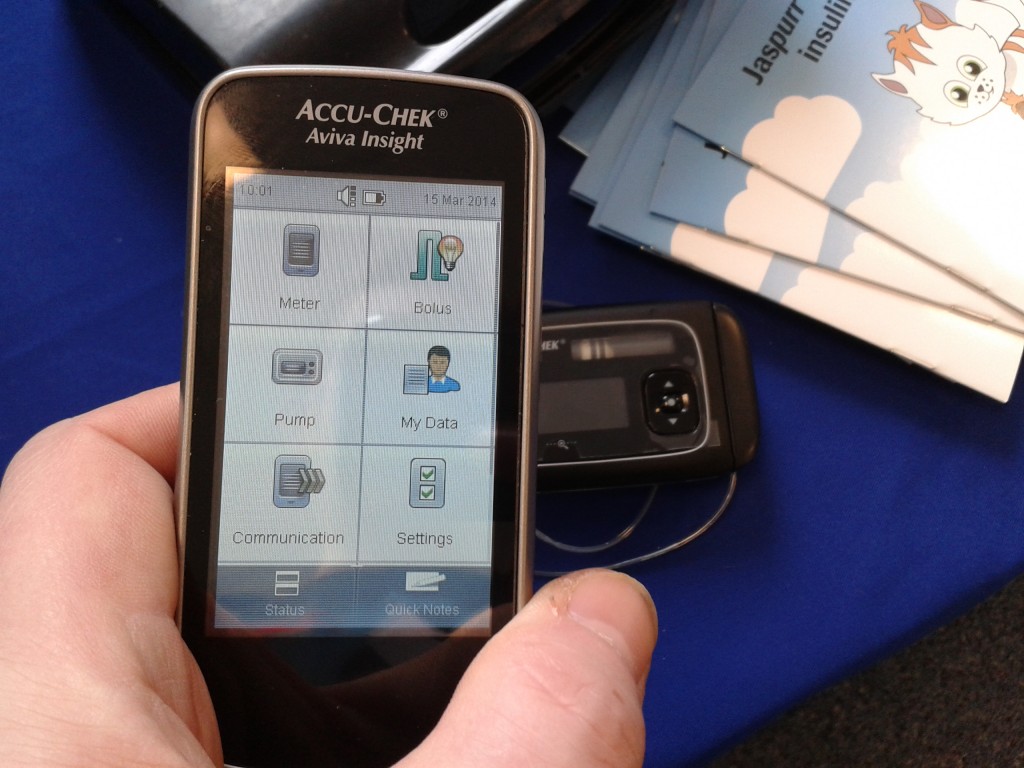
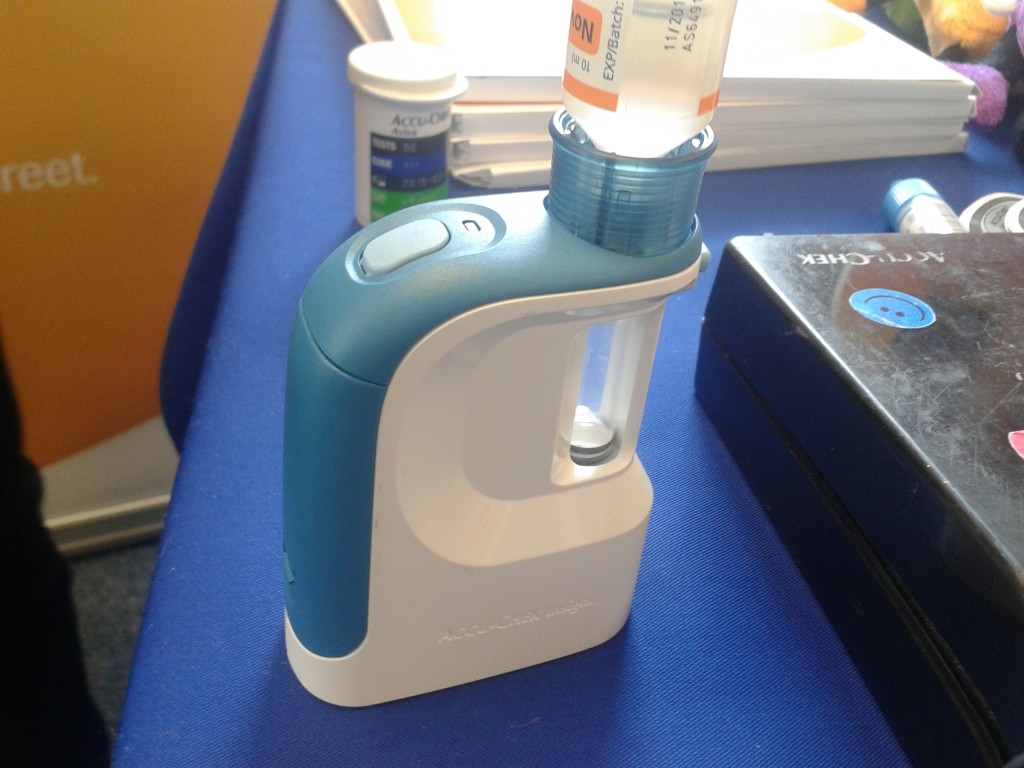
Post chat show and we shared some lunch with Partha – who arrived just as the session ended – and we discussed the event, how it went, questions that were asked. It was nice to talk about emerging technologies too, like the Abbott Flash Monitoring.
In the car Amy seemed disappointed, feeling she hadn’t done so well, remember getting tongue-tied on the first question, but she had done well and later I showed her some comments from people I’d never met before who saw this tweet: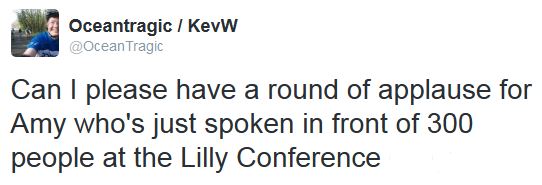
If you’re wondering whether the chat show format worked…
More importantly it was seen as a success in two ways. Firstly Amy went in at 8.7mmol, an hour later she was 8.7mmol (although then she ate evil pizza!). Secondly, this…




 I suppose the purchase of a non-diabetes-related
I suppose the purchase of a non-diabetes-related  From day one – okay it was probably more like day 101 – we tried to get Amy to be proud of her diabetes and not let it stop her achieving whatever she wanted. It’s a bold statement to make and one that on some days seems a mega-distance away but on the whole it’s achievable and spurs her and us on to do things that we probably wouldn’t have done if she’d never been diagnosed. It was around day 101 that we started planning our
From day one – okay it was probably more like day 101 – we tried to get Amy to be proud of her diabetes and not let it stop her achieving whatever she wanted. It’s a bold statement to make and one that on some days seems a mega-distance away but on the whole it’s achievable and spurs her and us on to do things that we probably wouldn’t have done if she’d never been diagnosed. It was around day 101 that we started planning our  On Saturday at a JDRF Discovery Day in Reading there was a
On Saturday at a JDRF Discovery Day in Reading there was a  Taking part in Gav’s GBR30/30 challenge made Amy even more determined to kick diabetes’ arse and it increased her advocacy for Diabetes. I see this in effect whenever we go to a diabetes event and someone sees her pump, which happened like clockwork at the JDRF event last Saturday. Amy had 6 or 7 adults and children all listening to every word she said as she described how having the pump has made life so much better for her and why it’s so ‘awesome’.
Taking part in Gav’s GBR30/30 challenge made Amy even more determined to kick diabetes’ arse and it increased her advocacy for Diabetes. I see this in effect whenever we go to a diabetes event and someone sees her pump, which happened like clockwork at the JDRF event last Saturday. Amy had 6 or 7 adults and children all listening to every word she said as she described how having the pump has made life so much better for her and why it’s so ‘awesome’. There’s no doubt that I find it difficult when occasionally it all becomes too much for Amy, those days when she’d rather just be someone with a fully functioning pancreas, those days when she doesn’t want to be different. I know she’s had too much when I just get ‘the look’ usually after I’ve asked her to try and fill out more details in her log book, which I use to check whether or not there’s a pattern and therefore her insulin pump’s basal needs adjusting. Just after I’ve got ‘the look’ I absolutely hate diabetes and wish it would bugger off for good. I normally don’t mention anything about diabetes for a good while afterwards.
There’s no doubt that I find it difficult when occasionally it all becomes too much for Amy, those days when she’d rather just be someone with a fully functioning pancreas, those days when she doesn’t want to be different. I know she’s had too much when I just get ‘the look’ usually after I’ve asked her to try and fill out more details in her log book, which I use to check whether or not there’s a pattern and therefore her insulin pump’s basal needs adjusting. Just after I’ve got ‘the look’ I absolutely hate diabetes and wish it would bugger off for good. I normally don’t mention anything about diabetes for a good while afterwards.
 image from http://mydavidcameron.com/
image from http://mydavidcameron.com/






 view the full article
view the full article






