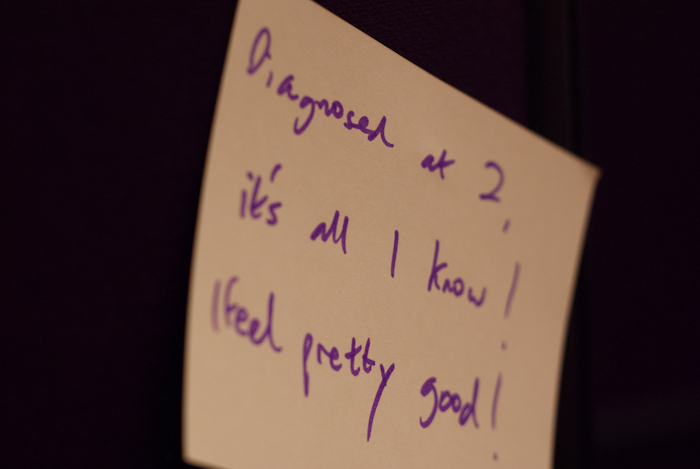
27 days after getting her insulin pump Amy went on her first European school trip, a two night stay in Koln, Germany.
Too soon after getting the pump?
When our DSN (Diabetes Specialist Nurse) called to let us know Amy would get her pump on the 20th June I was elated, before seconds later I remembered about her school residential trip to Germany, which was only a few weeks after. The DSN didn’t seem too worried though as long there was a clear 3 weeks before the trip – there was. This meant that Amy had to go straight on insulin when getting the pump, rather than spend a week using saline which some clinics do to get people used to using their new pump. Our DSNs confidence made us confident.
Amy would need to do a set change during the trip so would 27 days be enough to get used to doing this? By herself? Without us?
Negative press = worrying parents. Would the school still let her go?
In the news recently there’d been so many instances of kids being refused residential trips at the last minute that I attended a Parents’ Clinic run by the school, deciding to tackling this straight on.
I went in armed with articles such as ‘Sheffield schoolgirl with diabetes barred from trip‘ and ‘Diabetic lad is barred from school trip of a lifetime‘.
Their initial reaction was amazement, that schools would refuse to take kids with diabetes. I took that as a good sign.
Their official response came back a couple of days later: they just wanted a letter from the DSN a few days before the trip to say that Amy was fit to travel. They also wanted us to come in and discuss care requirements with the person who the designated pastoral carer for the trip.
The School’s Pastoral Carer
We already had great respect for Mrs L – the person assigned as the trip’s pastoral carer – as she’d helped our eldest daughter with some issues on her trip three years ago, so we were glad to hear she was going on this trip.
Jane went to meet her the day before the trip with a list of things to do, which featured a key message: you should not need to do anything except make sure she’s okay; you don’t need to inject her; you don’t need to touch her pump.
I felt it was important – after the articles I’d seen elsewhere – that the school didn’t feel like it would be a chore taking Amy on a trip and I didn’t want Amy to think that she needed to rely on others to manage her diabetes, which in turn would hopefully give her confidence. In general this worked very well, a few issues aside.
Three weeks to get the basal profile sorted
The DSN wanted 3 weeks between getting the pump and the trip so that adjustments could be made to Amy’s basal profile to get it right.
In turned out that 3 weeks was enough to get the basal profile as close as possible and more importantly make us confident enough to make slight tweaks ourselves.
Wednesday 17th July, Day one
Waking up at Stupid O’Clock
The coach was leaving at 4am. which mean at 3:30am wake up call. It also meant there was no chance of doing a set change that early in the morning, so one was done the afternoon before, with another one to be done on either Thursday on Friday, by Amy.
We knew that Amy’s basal profile was pretty good so didn’t feel the need for her to test her blood glucose level at such an ungodly hour.
Arriving at the school, there was a mix of excitement from the kids and anxiousness from the parents. They felt like I did three years ago when I packed my eldest off on the same trip. I found it hard to appreciate their fears considering everything we were now worrying about: if it all went wrong it literally could be life or death.
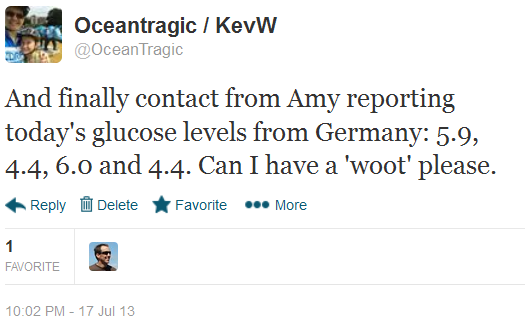
Still, I made sure Amy had her mobile so she could text me her blood glucose check results and ask for advice if needed. It was a long wait.
Diabetes? Here? Nah!
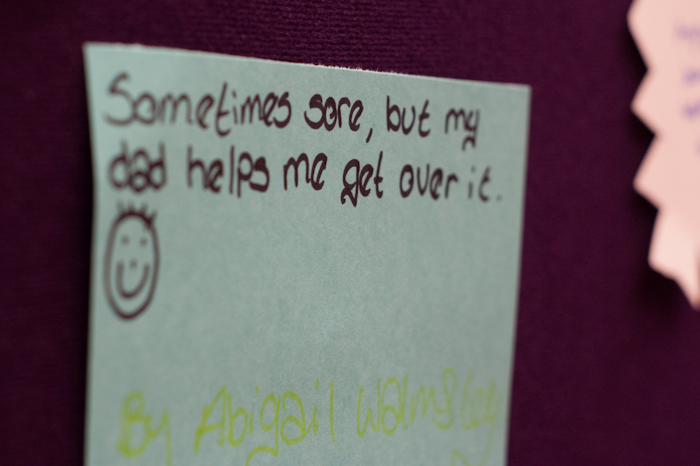
A key thing any parent would want for their kid on a school trip is that diabetes doesn’t feature very highly so we told Amy to enjoy herself, get the most of the the trip but keep safe.
And she did.
Whilst she never texted me her results until a lot later in the day she clearly felt in control enough to not need to call me either, which was great, if not a little concerning for an incommunicado parent.
Later in the evening she sent her BG results through:
Thursday 18th July, Day two
Lindt and excercise
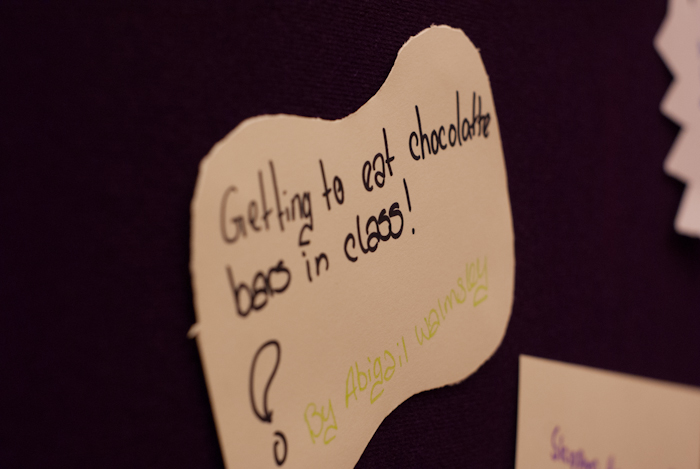
Today was the day which worried me most: it started off with a visit to the Lindt chocolate factory and also featured a lot of walking and a climb up Koln Cathedral’s 509 step spiral staircase.
We exchanged a few early morning texts one of which from Amy contained ‘is it okay if I have some chocolate at the Lindt factory?’. Bless her, as if I’d say no, knowing that she’d been looking forward to this specific visit for months. I looked up some nutritional values on Lindt’s informative web site and text Amy back carb values for stuff she likes. At Lindt she bolused three times in the space of the hour long visit, something she would never have done with injections so YAY for the pump, it meant she really enjoyed the visit.
The Koln Cathedral visit didn’t provide any problems either.
Infusion set change – without us
Amy had done all of the set changes herself, without us doing anything but with us watching and encouraging. Before the trip she wasn’t fazed about doing the set change and unsurprisingly she did it without issue, but under the close eye of the school’s Pastoral Carer.
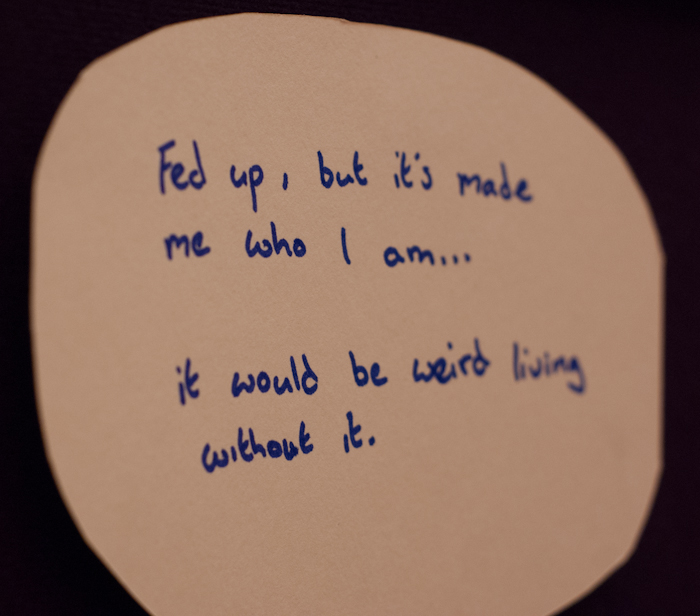
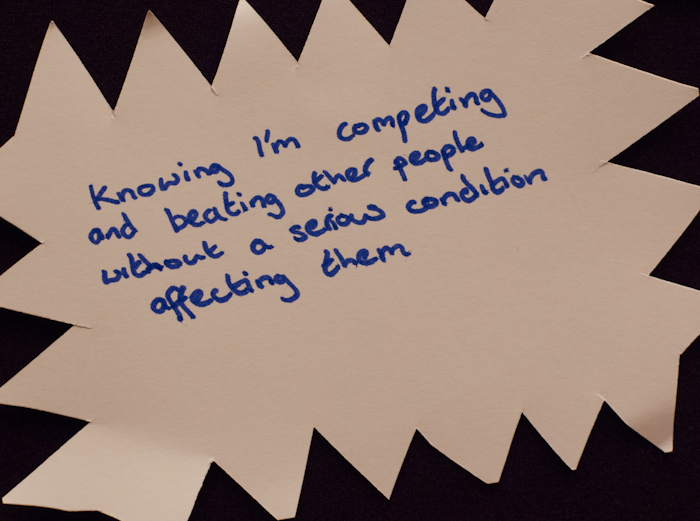
Count the boluses
I’ve said before that Amy hated injections so wouldn’t often choose to snack anything over 15g carbs, and even then only once between meals. So the pump has given her the ability to do this but maybe, just maybe, 10 boluses in a day is a little too much. Well actually no, it isn’t, everyone else was snacking and now Amy’s pump meant she could too, without worrying about soaring or dropping levels.
Today’s blood glucose levels
7.8, 14.9, 4.6, 8.3, 4.1, 5.1, 3.5, 5.9.
We can discount the 14.9 pre-lunch test as it was 70 minutes after the first Lindt chocolate and 20 minutes after the last.
This means she only went a maximum of 0.5 out of range all day.
I’d call that winning.
Friday 19th July, Day three
A morning of stress induced highs
This morning she’d woken at 6.6mmol, another great result.
The trip had been going so well for Amy, she was having fun and her levels were pretty great all round. Diabetes itself wasn’t getting in her way at all.
That was until it was time to pack up and one of her room mates got all stroppy and pushed the other room mate into a wall, causing an untold amount of stress and emotion. I wasn’t surprised to hear about this event as I’ve never understood why Amy is friends with this girl, she’s always be horrid to Amy, so why share a room with her? The other girl has been one of Amy’s closest friends forever and one we very much trust to look out for Amy.
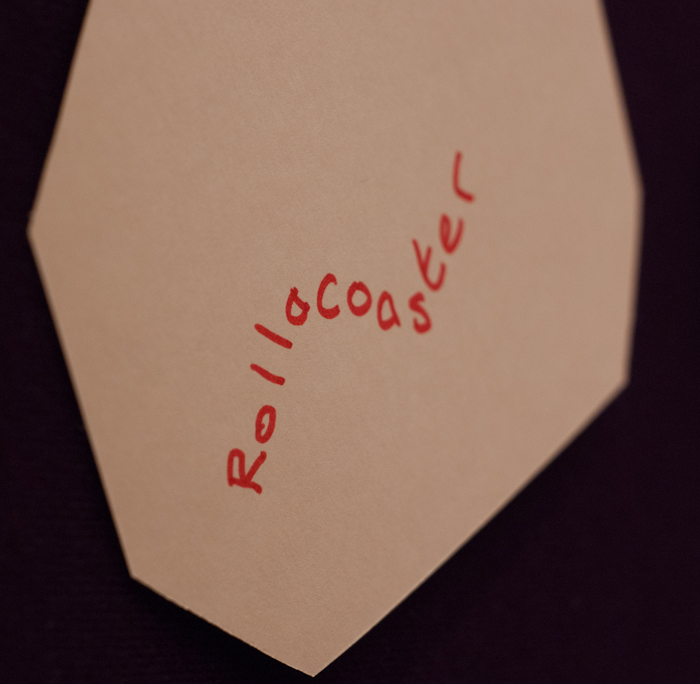
I was surprised how the stress affected Amy’s levels, shooting up to 15.5 which took a couple of corrections to shift over the next few hours.
By 1pm she was down to a respectable 5.4mmol.
Amy, do you really need Pizza for lunch?
The kids had to buy their own food on the last day, all opting for Pizza. I knew that a combo-bolus would be required but we don’t eat Pizza much at home and hadn’t experimented with combo -boluses for it. She wasn’t keen but I managed to convince Amy to do a four-hour bolus; I knew it needed to be longer but not when she’s by herself in Germany. We decided we’d run the risk of being higher later on…oh how that came back to bite us.
The case of the too-short-combo-bolus, the coach trip and the over-zealous teacher
Following Amy’s Pizza was the long coach journey back to England, sitting aimlessly on a coach for hours and hours. Combine this with the pizza and it’s easy to understand why Amy’s BG readings went up to 13.9.
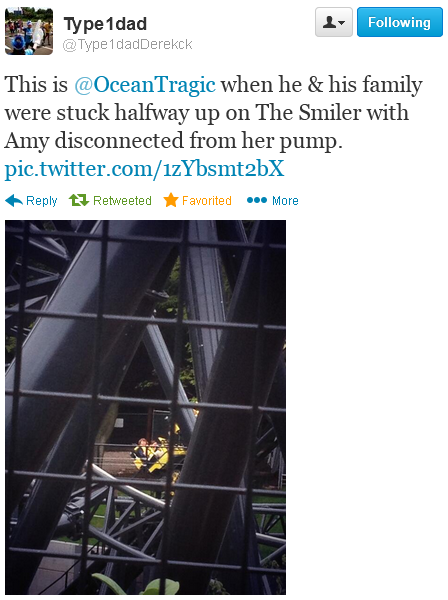
What we didn’t expect though was the lovely Pastoral Carer going a bit overboard. She got Amy to test for ketones and even though it was very low she got her to test again minutes later. Then another blood test, then another, then another.
She did 9 blood glucose tests within 3 hours and a few ketones tests too!
Clearly this was down to us not clearly communicating what Amy needed to do if high; we’d concentrated on the lows, not the highs. We’d spoken about ketone testing but somewhere the hypo-15-minute-rule and ketone testing rule got mixed up. For the record, I’d rather had an over-zealous teacher than one who didn’t care or check on Amy.
It clearly threw Amy off balance and made her panic a little, which in turn probably raised her levels higher. Since, we’ve had a chat about why she went high which has renewed her confidence in her management of her diabetes.
In short…
Friendship incidents aside, pizza bolusing aside, everything went perfectly for Amy. Diabetes never got in her way, or stopped her from doing anything, she did everything her friends did.




 Diabetes Research & Wellness Foundation
Diabetes Research & Wellness Foundation






 Announcement of new blog, November 2012
Announcement of new blog, November 2012 Excerpt by Dr Kar, Roche Reach magazine, Winter 2013
Excerpt by Dr Kar, Roche Reach magazine, Winter 2013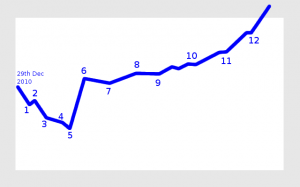 My view of our diabetes journey
My view of our diabetes journey

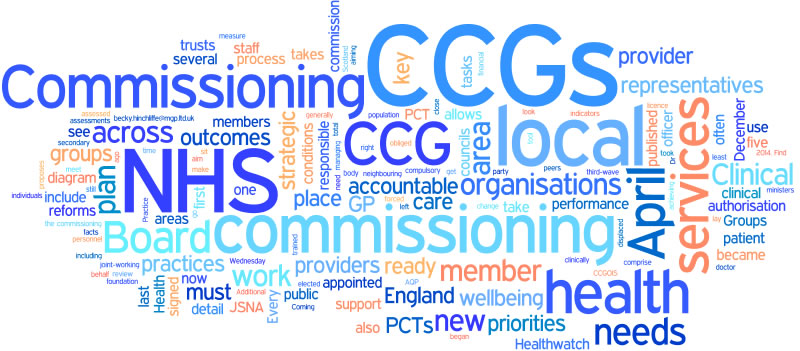
 Download my “How social media helps us with Type 1 Diabetes” leaflet
Download my “How social media helps us with Type 1 Diabetes” leaflet
 An HbA1c checking machine
An HbA1c checking machine
 Zoe welcomed us all to event, thanked us for coming and spoke a little about Hedgie Pricks Diabetes and today’s event and the speakers who we’d see later.
Zoe welcomed us all to event, thanked us for coming and spoke a little about Hedgie Pricks Diabetes and today’s event and the speakers who we’d see later.